Review of the Medical Literature
INTRODUCTION: Scientific understanding on the 'causes of depression' has changed
dramatically in recent years.
Once thought to result only from an imbalance of serotonin or psychological factors,
depression is now linked to
many abnormalities including 'leakiness' of the blood brain barrier - inflammation of
the brain - lack of
neurogenesis - autoimmunity toward neurons and synapses - high blood levels of
Interleukin 6 -
low levels of the brain hormone BDNF - and
an intestinal barrier defect known as 'leaky gut' (which allows toxic bacteria into the
blood).
Sparking great interest in recent years, severe disturbances of
the 10 trillion beneficial bacteria in the small and large intestine (known as the
microbiome) are now well documented in those with depression
(and an exciting area of treatment research). Not coincidentally,
the metabolites produced by microbiome bacteria are essential for the proper function
and
repair of the above mentioned physiology.
The exciting takeaway from this - now that the real causes of depression and anxiety are
being uncovered, it becomes possible
to treat and reverse these conditions in ways that were not possible even a few years
ago.
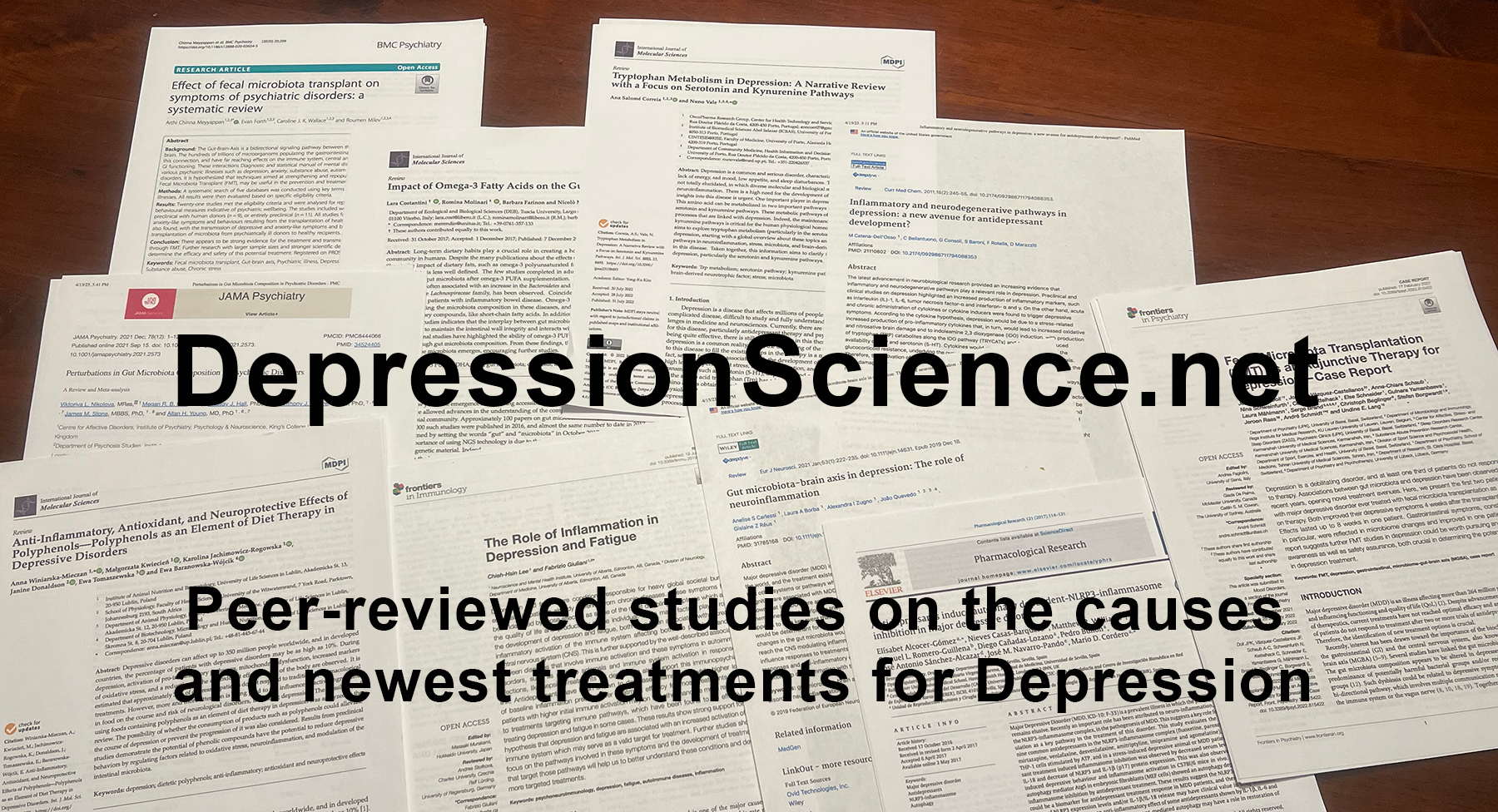
Our purpose at DS is to track-down and report the latest peer-reviewed studies on
unrecognized environmental
and dietary factors causing severe changes in the human brain and body over time, which
in turn, lead to depression and anxiety.
In our 'Treatments' section, we summarize the most promising and exciting new treatments
being investigated by universities around the globe,
with several showing astounding levels of success in treating and even erasing
depression.
As the majority of information in this medical review is new, and often contradictory to
older previously held opinions, you'll find these studies
not only exciting, but offer tremendous hope with immediate and easy to implement
strategies for reversing depression in children and adults alike.
...
.
With current antidepressant therapy said to benefit only 20-37% of patients, it's
certainly time to look deeper into alternatives.
In summary, medical science has only recently reached the point where it now has the
knowledge and ability to reverse and prevent
the rising rates of depression, anxiety and many other neurological disorders.
At DepressionScience.net, we've made it easy for professionals, patients and friends
to stay on top of the latest science on the causes and
treatments for depression.
Our summaries are carefully written to take often complex medical biology
and make it easy to understand by anyone of any age and backgrounds.
Not only do we review past publications,
but we search the National Library of Medicine database for new publications daily
in this rapidly changing field of neurology.
Links are provided to each peer-reviewed study making this an excellent
resource for both patients and professionals.
Unfortunately, this information has previously been inaccessible to patients and
unknown
to treating physicians.
We are also skilled at using cross-referencing to combine findings from two
different studies to reach new conclusions.
For example, a recent study was published showing COVID-19 infection increases
depression because of
the virus' ability to attach to ACE2 receptors common on the exterior of brain
cells.
We also have studies showing how various plant polyphenols can also attach to ACE2
and block viral attachment.
This would suggest that the consumption of various plant polyphenols
could be used in the treatment of COVID-19 induced depression.
This connection would normally be missed, but not by us.
All studies are peer-reviewed from the NIH National Library of Medicine database.
Each post includes a summary of the journal article as well as the journal name -
research centers involved - and a screen shot of the first page with journal
Abstract. Links to
the original study and downloadable PDF are also included. A checkbox is visible in
each
post. When this is selected, the first page of the journal article is SAVED and
added to your
own personal PDF Booklet. You can then choose to combine all title pages into a PDF
packet,
which can then be SAVED to your Desktop or Printed on the spot. Also, please
consider signing up for
our email notifications so you will be notified immediately when we upload a new
medical journal summary of interest.
Your email information remains private and is never shared with others.
...
.
With current antidepressant therapy said to benefit only 20-37% of patients,
it's certainly time to look deeper into alternatives.
In summary, medical science has only recently reached the point where it now has
the knowledge and ability to reverse and prevent
the rising rates of depression, anxiety and many other neurological disorders.
At DepressionScience.net, we've made it easy for professionals, patients and
friends to stay on top of the latest science on the causes and
treatments for depression.
Our summaries are carefully written to make take often complex medical biology
and make it easy to understand by anyone of any age and backgrounds.
Not only do we review past publications,
but we search the National Library of Medicine database for new publications
daily in this rapidly changing field of neurology.
Links are provided to each peer-reviewed study making this an excellent
resource for both patients and professionals.
Unfortunately, this information has previously been inaccessible to patients and
unknown
to treating physicians.
We are also skilled at using cross-referencing to combine findings from two
different studies to reach new conclusions.
For example, a recent study was published showing COVID-19 infection increases
depression because of
the virus' ability to attach to ACE2 receptors common on the exterior of brain
cells.
We also have studies showing how various plant polyphenols can also attach to
ACE2 and block viral attachment.
This would suggest that the consumption of various plant polyphenols
could be used in the treatment of COVID-19 induced depression.
This connection would normally by missed, but not by us.
All studies are peer-reviewed from the NIH National Library of Medicine
database.
Each post includes a summary of the journal article as well as the journal name
-
research centers involved - and a screen shot of the first page with abstract.
Links to
the original study and downloadable PDF are also included. A checkbox is visible
in each
post. When this is selected, the first page of the journal article is SAVED and
added to your
own personal PDF Booklet. You can then choose to combine all title pages into a
PDF packet,
which can then be SAVED to your Desktop or Printed on the spot. Also, please
consider signing up for
our email notifications so you will be notified immediately when we upload a new
medical journal summary of interest.
Your email information remains private and is never shared with others.
What's different in the brain or body of someone with depression? Researchers have recently identified major biological differences, far beyond just low serotonin. This section reviews the latest studies identifying elevated brain inflammation, higher inflammatory markers in the blood, increased autoimmunity, lack of new brain cell growth in the hippocampus (neurogenesis), weaker antioxidant defenses, leakage of toxins through the blood brain barrier and leakage of bacterial toxins through the gut barrier (leaky-gut). Also, recent discoveries have identified lower numbers of beneficial and higher disease causing bacteria in the gut microbiome of depressed patients. This new information provides pathways to dramatically improved treatment strategies as outlined in our 'Treatments' section.
March 10, 2024
Low birthweight increases risk of depression 21%
Dept of Biostat & Epidemiology, University of Massachusetts
Source: J Developmental Orig Health Diseases, Oct 2023
ABSTRACT
An individual's birthweight, a marker of in utero exposures, was recently associated with certain psychiatric conditions. However, studies investigating the relationship between an individual's preterm birth status and/or birthweight and risk for depression during adulthood are sparse; we used data from the Women's Health Initiative (WHI) to investigate these potential associations. At study entry, 86,925 postmenopausal women reported their birthweight by category (<6 lbs., 6-7 lbs. 15 oz., 8-9 lbs. 15 oz., or ≥10 lbs.) and their preterm birth status (full-term or ≥4 weeks premature). Women also completed the Burnham screen for depression and were asked to self-report if: (a) they had ever been diagnosed with depression, or (b) if they were taking antidepressant medications. Linear and logistic regression models were used to estimate unadjusted and adjusted effect estimates. Compared to those born weighing between 6 and 7 lbs. 15 oz., individuals born weighing <6 lbs. (βadj = 0.007, P < 0.0001) and ≥10 lbs. (βadj = 0.006, P = 0.02) had significantly higher Burnam scores. Individuals born weighing <6 lbs. were also more likely to have depression (adjOR 1.21, 95% CI 1.11-1.31). Individuals born preterm were also more likely to have depression (adjOR 1.18, 95% CI 1.02-1.35); while attenuated, this association remained in analyses limited to only those reportedly born weighing <6 lbs. Our research supports the role of early life exposures on health risks across the life course. Individuals born at low or high birthweights and those born preterm may benefit from early evaluation and long-term follow-up for the prevention and treatment of mental health outcomes.
February 14, 2024
Defective Blood Brain Barrier in depressed patients
Dept of Lab Med, All India Inst of Med Sci, India
Source: Indian Journal of Psychiatry, Jan-Feb 2019
ABSTRACT
Background:
The biochemical basis of depression has been related to blood–brain barrier (BBB) allowing/restricting a number of components to enter the brain milieu from the peripheral plasma milieu. S100B has been associated with BBB damage and is used as a marker of its integrity. Several studies have reported that depressive patients have increased levels of S100B in serum and cerebrospinal fluid.
Materials and Methods:
Forty-two confirmed cases of depression, 13–25 years of age were recruited from the Department of Psychiatry, All India Institute of Medical Sciences during the period from January 2013 to June 2014 along with 42 healthy controls of comparable age and sex. Psychometric evaluation of the patients and controls was done to assess the severity of depression using Beck's Depression Inventory-II and Hamilton Depression Rating Scale. Medical assessment and laboratory investigations were done. Serum S100B levels were measured using Sandwich ELISA. The results obtained were statistically analyzed.
Results:
Levels of serum S100B were significantly elevated in patients with major depression as compared to controls. Significantly higher levels of S100B were seen only in females as compared to their healthy counterparts. Serum S100B was higher in depressed participants with the recurrent disorder than those with single episode. No correlation of levels of this marker was seen with clinical severity of the patients. It was found that with increased duration of illness for which the patient was being treated with antidepressants, the patients had higher levels of S100B.
Conclusions:
Serum S100B can be used as a biomarker of depression.
February 11, 2024
Abnormal microbiome in depressive disorder
Nishtar Medical University, Pakistan
Source: Frontiers in Behavioral Neuroscience, Jun 2023
When comparing the gut microbiota of unmedicated people with major depressive disorder (MDD), people with bipolar disorder, and healthy controls, Zheng et al. (2020) conclude that there are differences between the groups. This research had two groups of controls: one was similar to the study participants regarding the aforementioned demographic factors, while the other was not. The gut microbiota of MDD patients differed from that of controls with the same age, gender, and body mass index. There were more Enterobacteriaceae and Alistipes in MDD patients’ guts and fewer Faecalibacterium, Coprococcus, and Dialister. Individuals with MDD had their gut microbiota studied. In addition to this, they found that only Pseudomonadaceae levels were higher in subjects diagnosed with bipolar disorder when compared to healthy controls. A signature of 26 operational taxonomic units (OTUs) was found to be needed to tell major depressive disorder (MDD) apart from bipolar disorder and healthy controls. Four of the 26 microbial OTUs were significantly linked to the Hamilton Depression Rating Scale (HAMD) in people with major depressive disorder or bipolar disorder (Zheng et al., 2020). Most of these were from the family Lachnospiraceae. The optimal conditions for a healthy microbiota community in the gut can be better understood by conducting research that also considers the effects of pharmacotherapy and diet.
...........................................................
ABSTRACT
The gut-brain axis is a communication pathway that allows a two-way exchange of information between the microbiota of the gastrointestinal tract and the nervous system of humans. The vagus nerve, which is responsible for facilitating communication, provides support for this axis. The gut-brain axis is currently the subject of research, but studies into the diversity and stratification of the gut microbiota are just getting started. Researchers have discovered several positive trends by analyzing numerous studies examining the gut microbiota’s impact on the effectiveness of SSRIs. It is common knowledge that a specific group of measurable, microbial markers has been recognized as being present in the feces of individuals suffering from depression. Specific bacterial species are a common denominator among therapeutic bacteria used to treat depression. It can also play a role in determining the severity of disease progression. Evidence that selective serotonin reuptake inhibitors (SSRIs) rely on the vagus nerve to exert their therapeutic effects has provided further support for the importance of the vagus nerve in the gut-brain axis, which is necessary for beneficial changes in the gut microbiota. This review will analyze the research linking gut microbiota to depression.
February 11, 2024
Beneficial gut bacteria low in patients with depression
Dept of Anatomy, Univ of Zurich, Switzerland
Source: Nutrients, Dec 2021
ABSTRACT
A growing number of studies in rodents indicate a connection between the intestinal microbiota and the brain, but comprehensive human data is scarce. Here, we systematically reviewed human studies examining the connection between the intestinal microbiota and major depressive and bipolar disorder. In this review we discuss various changes in bacterial abundance, particularly on low taxonomic levels, in terms of a connection with the pathophysiology of major depressive and bipolar disorder, their use as a diagnostic and treatment response parameter, their health-promoting potential, as well as novel adjunctive treatment options. The diversity of the intestinal microbiota is mostly decreased in depressed subjects. A consistent elevation of phylum Actinobacteria, family Bifidobacteriaceae, and genus Bacteroides, and a reduction of family Ruminococcaceae, genus Faecalibacterium, and genus Roseburia was reported. Probiotics containing Bifidobacterium and/or Lactobacillus spp. seemed to improve depressive symptoms, and novel approaches with different probiotics and synbiotics showed promising results. Comparing twin studies, we report here that already with an elevated risk of developing depression, microbial changes towards a "depression-like" microbiota were found. Overall, these findings highlight the importance of the microbiota and the necessity for a better understanding of its changes contributing to depressive symptoms, potentially leading to new approaches to alleviate depressive symptoms via alterations of the gut microbiota.
February 9, 2024
Blood brain barrier breakdown - neuroinflammation from DAMPS
Dept of Biochemistry and Molecular Medicine
Source: Journal of Neuroimmunology, Oct 2022
Although not discussed here, other studies have found an increasing number of endocrine disrupting chemicals (EDCs) can increase the release of DAMPS, thereby resulting in chronic low-grade inflammation and subtle neurological damage. The links here currently lead to the journal ABSTRACT. Once we acquire the full-version, links and text will be updated.
...........................................................
ABSTRACT
Depression is a heterogeneous mental disorder characterized by feelings of sadness and loss of interest that render the subject unable to handle basic daily activities such as sleeping, eating, or working. Neurobiological traits leading to depression include genetic background, early life abuse, life stressors, and systemic and central inflammatory profiles. Several clinical and preclinical reports documented that depression shows an increase in pro-inflammatory markers such as interleukin (IL-)1β, IL-6, IL-12, tumor necrosis factor (TNF), and interferon (IFN)-γ; and a decrease in anti-inflammatory IL-4, IL-10, and transforming growth factor (TGF)-β species. Inflammatory activation may trigger and maintain depression. Dynamic crosstalk between the peripheral immune system and the central nervous system (CNS) such as activated endothelial cells, monocytes, monocyte-derived dendritic cells, macrophages, T cells, and microglia has been proposed as a leading cause of neuroinflammation. Notably, pro-inflammatory cytokines disrupt the hypothalamic-pituitary-adrenal (HPA) axis and serotonergic, noradrenergic, dopaminergic, and glutamatergic neurotransmission. While still under investigation, peripheral cytokines can engage brain pathways and affect the central synthesis of HPA hormones and neurotransmitters through several mechanisms such as activation of the vagus nerve, increasing the permeability of the blood-brain barrier (BBB), altered cytokines transport systems, and engaging toll-like receptors (TLRs) by pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs). However, physiological mechanisms that favor time-dependent central inflammation before or during illness are not totally understood. This review will provide preclinical and clinical evidence of DAMPs and the BBB permeability as contributors to depression and neuroinflammation. We will also discuss pharmacologic approaches that could potentially modulate DAMPs and BBB permeability for future interventions against major depression.
February 4, 2024
Leaky gut causes neuroinflamation & depression
Dept of Psychiatry, Emory School of Medicine
Source: Current Psychiatry Reports, Sep 2019
ABSTRACT
Purpose of review: This article reviews the relationship of the microbiome, the gut-brain axis, and depression. It also will review factors which can influence this relationship, such as chronic stress, medications, and the Western diet typically consumed by adolescents.
Recent findings: Changes in the gut microbiome increase the release of microbial lipopolysaccharides (LPS) which activate a gut inflammatory response. Gut pro-inflammatory cytokines stimulate the afferent vagal nerve which in turn impacts the hypothalamic-pituitary-adrenal (HPA) axis inducing symptoms associated with depression. Recent research suggests that gut inflammation can induce neuroinflammation which, in turn, stimulates microglia activation and the kynurenine pathway and can activate systemic inflammation-inducing depressive symptoms. Promoting a healthy diet and lifestyle changes, limiting exposure to pesticides, limiting medications that affect the microbiome and the use of such things pre/probiotics and other interventions may complement existing efforts to curb the rise in depression. Alternative and complementary therapies may serve as effective treatments in adolescents with depression.
January 4, 2024
Brain derived neurotrophic factor (BDNF) - Time to learn
Dept Pharmacology, Ut Health San Antonio, TX
Source: World Journal of Psychiatry, Jan 2022
ABSTRACT
Major depressive disorder is a debilitating disorder affecting millions of people each year. Brain-derived neurotrophic factor (BDNF) and inflammation are two prominent biologic risk factors in the pathogenesis of depression that have received considerable attention. Many clinical and animal studies have highlighted associations between low levels of BDNF or high levels of inflammatory markers and the development of behavioral symptoms of depression. However, less is known about potential interaction between BDNF and inflammation, particularly within the central nervous system. Emerging evidence suggests that there is bidirectional regulation between these factors with important implications for the development of depressive symptoms and anti-depressant response. Elevated levels of inflammatory mediators have been shown to reduce expression of BDNF, and BDNF may play an important negative regulatory role on inflammation within the brain. Understanding this interaction more fully within the context of neuropsychiatric disease is important for both developing a fuller understanding of biological pathogenesis of depression and for identifying novel therapeutic opportunities. Here we review these two prominent risk factors for depression with a particular focus on pathogenic implications of their interaction.
December 15, 2023
Brain inflammation as cause of depression and loss of neurogenesis
Beijing Inst of Basic Medical Sciences
Source: Journal Neurinflammation, Nov 2023
ABSTRACT
As one of most common and severe mental disorders, major depressive disorder (MDD) significantly increases the risks of premature death and other medical conditions for patients. Neuroinflammation is the abnormal immune response in the brain, and its correlation with MDD is receiving increasing attention. Neuroinflammation has been reported to be involved in MDD through distinct neurobiological mechanisms, among which the dysregulation of neurogenesis in the dentate gyrus (DG) of the hippocampus (HPC) is receiving increasing attention. The DG of the hippocampus is one of two niches for neurogenesis in the adult mammalian brain, and neurotrophic factors are fundamental regulators of this neurogenesis process. The reported cell types involved in mediating neuroinflammation include microglia, astrocytes, oligodendrocytes, meningeal leukocytes, and peripheral immune cells which selectively penetrate the blood–brain barrier and infiltrate into inflammatory regions. This review summarizes the functions of the hippocampus affected by neuroinflammation during MDD progression and the corresponding influences on the memory of MDD patients and model animals.
December 12, 2023
Low defenses increase depressive disorder
Dept of Psychiatry, Jinan University, China
Source: PLoS One, Oct 7 2015
ABSTRACT
Object
Studies have suggested that depression was accompanied by oxidative stress dysregulation, including abnormal total antioxidant capacity (TAC), antioxidants, free radicals, oxidative damage and autoimmune response products. This meta-analysis aims to analyse the clinical data quantitatively by comparing the oxidative stress markers between depressed patients and healthy controls.
Methods
A search was conducted to collect the studies that measured the oxidative stress markers in depressed patients. Studies were searched in Embase, Medline, PsychINFO, Science direct, CBMDisc, CNKI and VIP from 1990 to May 2015. Data were subjected to meta-analysis by using a random effects model for examining the effect sizes of the results. Bias assessments, heterogeneity assessments and sensitivity analyses were also conducted.
Results
115 articles met the inclusion criteria. Lower TAC was noted in acute episodes (AEs) of depressed patients (p<0.05). Antioxidants, including serum paraoxonase, uric acid, albumin, high-density lipoprotein cholesterol and zinc levels were lower than controls (p<0.05); the serum uric acid, albumin and vitamin C levels were increased after antidepressant therapy (p<0.05). Oxidative damage products, including red blood cell (RBC) malondialdehyde (MDA), serum MDA and 8-F2-isoprostanes levels were higher than controls (p<0.05). After antidepressant medication, RBC and serum MDA levels were decreased (p<0.05). Moreover, serum peroxide in free radicals levels were higher than controls (p<0.05). There were no differences between the depressed patients and controls for other oxidative stress markers.
Conclusion
This meta-analysis supports the facts that the serum TAC, paraoxonase and antioxidant levels are lower, and the serum free radical and oxidative damage product levels are higher than controls in depressed patients. Meanwhile, the antioxidant levels are increased and the oxidative damage product levels are decreased after antidepressant medication. The pathophysiological relationships between oxidative stress and depression, and the potential benefits of antioxidant supplementation deserve further research.
April 19, 2023
MRI & PET imaging show brain inflammation
Emory Univ School of Med. Atlanta, GA
Source: Current Neuropharmacology, Jun 2018
Areas of the brain involved in fear, anxiety and threat detection were also thrown into abnormal balance after exposure to elevated inflammatory cytokines. Researchers place strong emphasis on the many studies showing brain inflammation causes reduced production of "monoamines" such as serotonin and dopamine.
............................................................
ABSTRACT
Studies investigating the impact of a variety of inflammatory stimuli on the brain and behavior have reported evidence that inflammation and release of inflammatory cytokines affect circuitry relevant to both reward and threat sensitivity to contribute to behavioral change. Of relevance to mood and anxiety-related disorders, biomarkers of inflammation such as inflammatory cytokines and acute-phase proteins are reliably elevated in a significant proportion of patients with major depressive disorder (MDD), bipolar disorder, anxiety disorders and post-traumatic stress disorder (PTSD).
Methods
This review summarized clinical and translational work demonstrating the impact of peripheral inflammation on brain regions and neurotransmitter systems relevant to both reward and threat sensitivity, with a focus on neuroimaging studies involving administration of inflammatory stimuli. Recent translation of these findings to further understand the role of inflammation in mood and anxiety-related disorders is also discussed.
Results
Inflammation was consistently found to affect basal ganglia and cortical reward and motor circuits to drive reduced motivation and motor activity, as well as anxiety-related brain regions including amygdala, insula and anterior cingulate cortex, which may result from cytokine effects on monoamines and glutamate. Similar relationships between inflammation and altered neurocircuitry have been observed in MDD patients with increased peripheral inflammatory markers, and such work is on the horizon for anxiety disorders and PTSD.
Conclusion
Neuroimaging effects of inflammation on reward and threat circuitry may be used as biomarkers of inflammation for future development of novel therapeutic strategies to better treat mood and anxiety-related disorders in patients with high inflammation.
April 18, 2023
Inflammation as cause of Depression
Division of Neurology, Univ of Alberta, CA
Source: Frontiers in Immunology, Jul 2019
ABSTRACT
Depression and fatigue are conditions responsible for heavy global societal burden, especially in patients already suffering from chronic diseases. These symptoms have been identified by those affected as some of the most disabling symptoms which affect the quality of life and productivity of the individual. While many factors play a role in the development of depression and fatigue, both have been associated with increased inflammatory activation of the immune system affecting both the periphery and the central nervous system (CNS). This is further supported by the well-described association between diseases that involve immune activation and these symptoms in autoimmune disorders, such as multiple sclerosis and immune system activation in response to infections, like sepsis. Treatments for depression also support this immunopsychiatric link. Antidepressants have been shown to decrease inflammation, while higher levels of baseline inflammation predict lower treatment efficacy for most treatments. Those patients with higher initial immune activation may on the other hand be more responsive to treatments targeting immune pathways, which have been found to be effective in treating depression and fatigue in some cases. These results show strong support for the hypothesis that depression and fatigue are associated with an increased activation of the immune system which may serve as a valid target for treatment. Further studies should focus on the pathways involved in these symptoms and the development of treatments that target those pathways will help us to better understand these conditions and devise more targeted treatments.
April 17, 2023
Higher inflammation markers in children predict future depression
Dept of Psychiatry, Univ of Cambridge, England
Source: JAMA Psychiatry, Oct 2014
4,500 children aged 9, were included in thE study. Childrens' blood was analyzed for the inflammatory markers C-Reactive Protein (CRP) and Interleukin-6 (IL-6). When children reached 18 years of age, their mental state was determined using the Mood & Feelings Questionnaire and records searched for psychotic disorders. Children who had higher inflammatory markers at age 9 were were 55% more likely to develop depression at age 18 and 140% more likely to have experienced a psychotic disorder. Researcers stated this provides evidence that inflammation is actually the cause of depression rather than occurring after someone has depression.
ABSTRACT
Longitudinal studies have linked the systemic inflammatory markers interleukin 6 (IL-6) and C-reactive protein (CRP) with the risk of developing heart disease and diabetes mellitus, which are common comorbidities for depression and psychosis. Recent meta-analyses of cross-sectional studies have reported increased serum levels of these inflammatory markers in depression, first-episode psychosis, and acute psychotic relapse; however, the direction of the association has been unclear.
OBJECTIVE
To test the hypothesis that higher serum levels of IL-6 and CRP in childhood would increase future risks for depression and psychosis.
DESIGN, SETTING, AND PARTICIPANTS
The Avon Longitudinal Study of Parents and Children (ALSPAC)is a prospective general population birth cohort study based in Avon County, England. We have studied a subsample of approximately 4500 individuals from the cohort with data on childhood IL-6 and CRP levels and later psychiatric assessments.
MEASUREMENT OF EXPOSURE
Levels of IL-6 and CRP were measured in nonfasting blood samples obtained in participants at age 9 years.
MAIN OUTCOMES AND MEASURES
Participants were assessed at age 18 years. Depression was measured using the Clinical Interview Schedule–Revised (CIS-R) and Mood and Feelings Questionnaire (MFQ), thus allowing internal replication; psychotic experiences (PEs) and psychotic disorder were measured by a semistructured interview.
RESULTS
After adjusting for sex, age, body mass index, ethnicity, social class, past psychological and behavioral problems, and maternal postpartum depression, participants in the top third of IL-6 values compared with the bottom third at age 9 years were more likely to be depressed (CIS-R) at age 18 years (adjusted odds ratio [OR], 1.55; 95% CI, 1.13-2.14). Results using the MFQ were similar. Risks of PEs and of psychotic disorder at age 18 years were also increased with higher IL-6 levels at baseline (adjusted OR, 1.81; 95% CI, 1.01-3.28; and adjusted OR, 2.40; 95% CI, 0.88-6.22, respectively). Higher IL-6 levels in childhood were associated with subsequent risks of depression and PEs in a dose-dependent manner.
CONCLUSIONS AND RELEVANCE
Higher levels of the systemic inflammatory marker IL-6 in childhood are associated with an increased risk of developing depression and psychosis in young adulthood. Inflammatory pathways may provide important new intervention and prevention targets for these disorders. Inflammation might explain the high comorbidity between heart disease, diabetes mellitus, depression, and schizophrenia.
As the percentage of children and young adults being diagnosed with depressive disorder (depression) has risen dramatically the past 20 years (over 7% yearly), researchers state this demonstrates environmental factors as the likely cause. This section reviews the latest studies investigating previously believed 'safe' circumstances in our lives are actually able to cause damage to the brain and its defenses over time, thereby increasing rates of depression. Upon understanding these circumstances, they can easily be avoided or reduced, thereby preventing depression onset or reversing symptom severity.
April 4, 2024
Traffic air pollution & flame retardant increased postpartum depression
Dept of Med & Surgery, University of Milan, Italy
Source: Journal of Clinical Medicine, Apr 2023
ABSTRACT
Background: The aim of the present study was to summarise the available data about the link between air pollution exposure and the new-onset and severity of psychiatric disorders in pregnant women during the perinatal period.
Materials and methods: We selected articles published until June 2022 on PubMed and the Web of Science. Pollutants included were PM2.5 (particulate matter 2.5 micrometres and smaller), PM10 (particulate matter 10 micrometres and smaller), NO2 (nitrogen dioxide), O3 (ozone), SO2 (sulphur dioxide), CO (carbon monoxide), PBDEs (polybrominated diphenyl ethers), PFAS (per- and polyfluoroalkyl substances), lead, and cadmium. The perinatal period was considered as the time of pregnancy until one year after childbirth.
Results: Nine studies were included; most of them evaluated the association between exposure to air pollutants and the onset of Postpartum Depression (PPD). Two studies showed an association between, respectively, only PM2.5 and both PM2.5 and NO2 exposure and PPD onset 12 months after childbirth, while another study found a significant association between NO2 exposure and PPD occurrence 6 months after childbirth. PBDE blood levels were associated with more severe depressive symptoms. Lastly, one study observed a link between stressful symptoms and exposure to PM2.5, PM10 during pregnancy.
Conclusion: More comprehensive and uniform studies are required to make a roadmap for future interventions, given the growing relevance of issues such pollution and mental health, particularly during the perinatal period.
March 10, 2024
In Vitro Fertilization (IVF) increases odds of future depression in offspring
Div of Obstetrics & Gynaecology, Univ of Western Australia
Source: Human Reproduction, Nov 2022
ABSTRACT
Study question: Does mental health and behaviour differ between those conceived with and those conceived without ART?
Summary answer: Our study observed less externalizing behaviour (delinquent/aggressive), and more parent-reported internalizing behaviour, as well as more (clinical) depression at age 14 years, in adolescents conceived after ART compared to their non-ART counterparts.
What is known already: Health outcomes of ART-conceived offspring may differ from those conceived without ART, and previous studies have reported differences in behaviour and mental health, particularly in childhood.
Study design, size, duration: The Growing Up Healthy Study (GUHS) is a prospective cohort study, investigating the long-term health of offspring conceived after ART (aged 14, 17 and 20 years), in the two operational fertility clinics in Western Australia 1991-2001 (n = 303). Their long-term health outcomes were compared to those of offspring conceived without ART from the Raine Study Generation 2 (Gen2) born 1989-1991 (n = 2868). Both cohorts are representative of the local adolescent population.
Participants/materials, setting, methods: Mental health parameters and behaviour were assessed at ages 14 and 17 years, through the parent completed 'Child Behaviour Checklist' (CBCL; ART versus non-ART: age 14 years: N = 150 versus N = 1781, age 17 years: N = 160 versus N = 1351), and the adolescent completed equivalent 'Youth Self-Report' (YSR; age 14 years: by N = 151 versus N = 1557, age 17 years: N = 161 and N = 1232). Both tools generate a T-score (standardized for age and sex) for internalizing (withdrawn, somatic complaints, anxious/depressed), externalizing (delinquent/aggressive behaviour) and total behaviour. Adolescents also completed the 'Beck Depression Inventory for Youth' (BDI-Y; age 14 years: N = 151 versus N = 1563, age 17 years: N = 161 versus N = 1219). Higher scores indicate poorer mental health and behaviour on all the above tools. Parent-reported doctor-diagnosed conditions (anxiety, behavioural problems, attention problems and depression) were also univariately compared between the cohorts. In addition, univariate comparisons were conducted between the GUHS adolescents and Gen2 adolescents born to subfertile parents (time to pregnancy >12 months), as well as between offspring born to subfertile versus fertile parents within the Gen2 cohort. A subgroup analysis excluding offspring born preterm (<37 weeks' gestation) or at low birthweight (<2500 g) was also performed. Generalized estimating equations that account for correlated familial data were adjusted for the following covariates: non-singleton, primiparity, primary caregiver smoking, family financial problems, socio-economic status and both maternal and paternal ages at conception.
Main results and the role of chance: At both 14 and 17 years of age, ART versus non-ART-conceived adolescents reported lower mean T-scores for externalizing problems (age 14 years: 49 versus 51, P = 0.045, age 17 years: 49 versus 52, P < 0.001). A similar effect was reported by parents, although not significant (age 14 years: P = 0.293, age 17 years: P = 0.148). Fewer ART-conceived adolescents reported a T-score above the clinical cut-off for externalizing behaviour (≥60; age 14 years: 7.3% versus 16.3%, P = 0.003, age 17 years: 8.1% versus 19.7%, P < 0.001). At both ages, no differences in internalizing behaviour were reported by adolescents (age 14 years: P = 0.218, age 17 years: P = 0.717); however, higher mean scores were reported by parents of the ART-conceived adolescents than by parents of the non-ART conceived adolescents (age 14 years: 51 versus 48, P = 0.027, age 17 years: 50 versus 46, P < 0.001). No differences in internalizing behaviour above the clinical cut-off (T-score ≥ 60) were observed. At age 17 years, parents who conceived through ART reported higher total behaviour scores than those parents who conceived without ART (48 versus 45, P = 0.002). At age 14 years, ART versus non-ART-conceived adolescents reported significantly higher mean scores on the BDI-Y (9 versus 6, P = 0.005); a higher percentage of adolescents with a score indicating clinical depression (≥17; 12.6% versus 8.5%, aOR 2.37 (1.18-4.77), P = 0.016), as well as more moderate/severe depression (≥21; 9.3% versus 4.0%, P = 0.009). At age 17 years, no differences were reported on the BDI-Y. There was also a higher percentage of parent-reported doctor-diagnosed anxiety in the ART cohort (age 14 years: 8.6% versus 3.5%, P = 0.002, at age 17 years: 12.0% versus 4.5%, P < 0.001). Removing adolescents born preterm or at low birthweight did not alter the above results. Comparing outcomes between GUHS adolescents and Gen2 adolescents born to subfertile parents, as well as between those born to subfertile versus fertile parents within Gen2, did not alter results for CBCL and YSR outcomes. Those born to subfertile parents showed higher rates of clinical depression than those born to fertile parents at age 14 years (13.7% versus 6.9%, P = 0.035).
Limitations, reasons for caution: The main limitation of the study is the time difference between the GUHS and Gen2 assessments. Even though we have adjusted for covariates, additional socio-economic and lifestyle factors affecting behaviour and mental well-being could have changed. We were unable to differentiate between different types of ART (e.g. IVF versus ICSI), owing to the low number of ICSI cycles at the time of study. Fertility sub-analyses need to be replicated in larger cohorts to increase power, potentially using siblingship designs. Lastly, selection bias may be present.
Wider implications of the findings: The reported lower prevalence of externalizing behaviour (delinquent/aggressive), and higher prevalence of internalizing behaviour, as well as more (clinical) depression at age 14 years, in ART versus non-ART-conceived adolescents, is in line with some previous studies, mostly conducted in childhood. It is reassuring that differences in the rates of depression were not observed at age 17 years, however, these findings require replication. As the use of ART is common, and mental health disorders are increasing, knowledge about a potential association is important for parents and healthcare providers alike.
March 7, 2024
BPA during pregnancy increases child depression
Columbia Ctr for Children's Env Health, Columbia University
Source: Environmental Research, Nov 2016
BPA was also shown to bind onto testosterone receptors, resulting in decreased testosterone levels. As shown in this 2017 study from China, BPA exposure decreased the number of Serotoli cells in the testicles, which are responsible for sperm production. The study on BPA reducing testosterone can seen from this link.
ABSTRACT
Background
Experimental and epidemiological studies suggest that gestational exposure to Bisphenol A (BPA), an ubiquitous endocrine disrupting chemical, may lead to neurobehavioral problems in childhood; however, not all results have been consistent. We previously reported a positive association between prenatal BPA exposure and symptoms of anxiety/depression reported by the mother at child age 7–9 years in boys, but not girls.
Objectives
Here, in the same birth cohort, we investigated the association of prenatal BPA exposure with symptoms of depression and anxiety self-reported by the 10–12 year olds, hypothesizing that we would observe sex-specific differences in anxiety and depressive symptoms.
Methods
African-American and Dominican women living in Northern Manhattan and their children were followed from mother’s pregnancy through children’s age 10–12 years. BPA was quantified in maternal urine collected during the third trimester of pregnancy and in child urine collected at ages 3 and 5 years. Children were evaluated using the Revised Children’s Manifest Anxiety Scale (RCMAS) and Children’s Depression Rating Scale (CDRS). We compared the children in the highest tertile of BPA concentration to those in the lower two tertiles. Associations between behavior and prenatal (maternal) BPA concentration or postnatal (child) BPA concentration were assessed in regression models stratified by sex.
Results
Significant positive associations between prenatal BPA and symptoms of depression and anxiety were observed among boys. Postnatal BPA exposure was not significantly associated with outcomes. There was substantial co-occurrence of anxiety and depressive symptoms in this sample.
Conclusion
These results provide evidence that prenatal BPA exposure is associated with more symptoms of anxiety and depression in boys but not in girls at age 10–12 years.
February 29, 2024
Ultra Processed Foods increase depression 22%
School of Medicine, Deakin University, Australia
Source: British Medical Journal, 2024
According to the Harvard Health Blog - ultra prcoessed foods
are most likely to have many added ingredients such as sugar, salt, fat, and artificial colors or preservatives. Ultra-processed foods are made mostly from substances extracted from foods, such as fats, starches, added sugars, and hydrogenated fats. They may also contain additives like artificial colors and flavors or stabilizers. Examples of these foods are frozen meals, soft drinks, hot dogs and cold cuts, fast food, packaged cookies, cakes, and salty snacks.
ABSTRACT
Objective To evaluate the existing meta-analytic evidence of associations between exposure to ultra-processed foods, as defined by the Nova food classification system, and adverse health outcomes.
Design Systematic umbrella review of existing meta-analyses.
Data sources MEDLINE, PsycINFO, Embase, and the Cochrane Database of Systematic Reviews, as well as manual searches of reference lists from 2009 to June 2023.
Eligibility criteria for selecting studies Systematic reviews and meta-analyses of cohort, case-control, and/or cross sectional study designs. To evaluate the credibility of evidence, pre-specified evidence classification criteria were applied, graded as convincing (“class I”), highly suggestive (“class II”), suggestive (“class III”), weak (“class IV”), or no evidence (“class V”). The quality of evidence was assessed using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) framework, categorised as “high,” “moderate,” “low,” or “very low” quality.
Results:
The search identified 45 unique pooled analyses, including 13 dose-response associations and 32 non-dose-response associations (n=9 888 373). Overall, direct associations were found between exposure to ultra-processed foods and 32 (71%) health parameters spanning mortality, cancer, and mental, respiratory, cardiovascular, gastrointestinal, and metabolic health outcomes. Based on the pre-specified evidence classification criteria, convincing evidence (class I) supported direct associations between greater ultra-processed food exposure and higher risks of incident cardiovascular disease related mortality (risk ratio 1.50, 95% confidence interval 1.37 to 1.63; GRADE=very low) and type 2 diabetes (dose-response risk ratio 1.12, 1.11 to 1.13; moderate), as well as higher risks of prevalent anxiety outcomes (odds ratio 1.48, 1.37 to 1.59; low) and combined common mental disorder outcomes (odds ratio 1.53, 1.43 to 1.63; low). Highly suggestive (class II) evidence indicated that greater exposure to ultra-processed foods was directly associated with higher risks of incident all cause mortality (risk ratio 1.21, 1.15 to 1.27; low), heart disease related mortality (hazard ratio 1.66, 1.51 to 1.84; low), type 2 diabetes (odds ratio 1.40, 1.23 to 1.59; very low), and depressive outcomes (hazard ratio 1.22, 1.16 to 1.28; low), together with higher risks of prevalent adverse sleep related outcomes (odds ratio 1.41, 1.24 to 1.61; low), wheezing (risk ratio 1.40, 1.27 to 1.55; low), and obesity (odds ratio 1.55, 1.36 to 1.77; low). Of the remaining 34 pooled analyses, 21 were graded as suggestive or weak strength (class III-IV) and 13 were graded as no evidence (class V). Overall, using the GRADE framework, 22 pooled analyses were rated as low quality, with 19 rated as very low quality and four rated as moderate quality.
Conclusions Greater exposure to ultra-processed food was associated with a higher risk of adverse health outcomes, especially cardiometabolic, common mental disorder, and mortality outcomes. These findings provide a rationale to develop and evaluate the effectiveness of using population based and public health measures to target and reduce dietary exposure to ultra-processed foods for improved human health. They also inform and provide support for urgent mechanistic research.
February 22, 2024
Alchohol increases depression by damaging critical defense
Dept of Internal Medicine, Rush Univ Medical Center, IL
Source: Alcohol Research, 2015
ABSTRACT
The excessive use of alcohol is a global problem causing many adverse pathological health effects and a significant financial health care burden. This review addresses the effect of alcohol consumption on the microbiota in the gastrointestinal tract (GIT). Although data are limited in humans, studies highlight the importance of changes in the intestinal microbiota in alcohol-related disorders. Alcohol-induced changes in the GIT microbiota composition and metabolic function may contribute to the well-established link between alcohol-induced oxidative stress, intestinal hyperpermeability to luminal bacterial products, and the subsequent development of alcoholic liver disease (ALD), as well as other diseases. In addition, clinical and preclinical data suggest that alcohol-related disorders are associated with quantitative and qualitative dysbiotic changes in the intestinal microbiota and may be associated with increased GIT inflammation, intestinal hyperpermeability resulting in endotoxemia, systemic inflammation, and tissue damage/organ pathologies including ALD. Thus, gut-directed interventions, such as probiotic and synbiotic modulation of the intestinal microbiota, should be considered and evaluated for prevention and treatment of alcohol-associated pathologies.
February 19, 2024
Common chemicals worsen postpartum depression and damage child neurodevelopment
College of Nursing Sci, Kyung Hee University, S. Korea
Source: Environ Sci Pollution Research Intl, Sep 2023
ABSTRACT
Exposure to endocrine-disrupting chemicals (EDCs) can promote infant neurodevelopmental impairment and maternal postpartum depression (PPD). However, the associations between lactation exposure to EDCs, maternal PPD, and infant neurodevelopment are unclear. Hence, we investigated these relationships in infants aged 36-42 months. We recruited 221 Korean mothers and analyzed 29 EDCs. The Edinburgh Postnatal Depression Scale (EPDS) was used to assess maternal PPD. Bayley scales of infant development; the Swanson, Nolan, and Pelham rating scale (SNAP); and the Child Behavior Checklist (CBCL) were used to assess neurodevelopment in infants exposed to the top 30% of EDC over three years. Multiple regression analyses were adjusted for maternal age, pre-pregnancy body mass index, education, income, employment, residence, and infant age and sex. The rates of infants with clinically abnormal diagnoses on neurologic developmental tests (Balyey, SNAP, and CBCL scales) ranged from 7.7 to 38.5% in this study, with the motor and hyperactivity/impulsivity areas scoring the highest among 65 boys and girls. Mono-2-ethylhexyl phthalate (MEHP) and mono-isononyl phthalate (MiNP) levels in breast milk significantly correlated with infant inattention and hyperactivity. Perfluorononanoic acid (PFNA) and perfluorooctyl sulfonate (PFOS) levels correlated significantly with motor development of BSID-III and total CBCL score which mean infant might have lower developmental status. EDC concentrations in breast milk were not associated with maternal PPD. Overall, lactational exposure to EDCs during the postpartum period can exert a negative effect on maternal PPD and infant neurodevelopment.
February 19, 2024
Persistent depression predicted by continuous low grade inflammation
Dept of Epidem & Public Health, University College London
Source: Psychopharmacology, 2016
At the end of the study period, researchers stated that higher levels of IL-6 and CRP predicted persistent depression and severity (as shown on the CES-D test), with higher IL-6 being a more accurate predictor of higher CES-D test scores. This study adds further evidence that inflammation is a highly significant contributor to depression. As more environmental and dietary factors are being shown in other studies to increase IL-6 and/or CRP, this strongly suggests their avoidance could quickly reduce depression and improve mental function.
...........................................................
ABSTRACT
Rationale
Evidence suggests that depression is cross-sectionally and longitudinally associated with activation of inflammatory response system. A few studies, however, have investigated the longitudinal relationship between raised inflammatory biomarkers and persistence of depressive symptoms. We examined the temporal relationship between serum levels of inflammatory biomarkers and persistence of depressive symptoms among older participants.
Methods
Center for Epidemiologic Studies Depression Scale (CES-D) was used to assess depressive symptoms at baseline and at 5-year follow-up in 656 participants (233 men, 423 women) aged >60 years of the Rotterdam Study. Markers of inflammation interleukin (IL)-6, alpha-1-antichymotrypsin (ACT) and C-reactive protein (CRP) were assessed at baseline, and all participants taking antidepressant medications were excluded from the analysis.
Results
No cross-sectional association was found between IL-6, ACT and CRP with depressive symptoms at baseline. However, higher levels of IL-6 and CRP predicted depressive symptoms at 5-year follow-up. Adjustment for confounding variables had no impact on the observed associations. Similarly, a positive association was found between baseline levels of IL-6 (OR = 2.44, p = 0.030) and CRP (OR = 1.81, p = 0.052) and persistence of depressive symptoms over 5 years.
Conclusion
Our data suggest that dysregulation of the inflammatory response system is associated with a more severe form of depression more likely to re-occur.
February 18, 2024
MSG & Aspartame reduce serotonin, dopamine & glutathione
Dept of Biology, Dammam Univ, Saudi Arabia
Source: Nerotoxicology Teratology, Mar-Apr 2014
The present study was designed to investigate the in vivo effects of monosodium glutamate (MSG) and aspartame (ASM) individually and in combination on the cognitive behavior and biochemical parameters like neurotransmitters and oxidative stress indices in the brain tissue of mice. Forty male Swiss albino mice were randomly divided into four groups of ten each and were exposed to MSG and ASM through drinking water for one month. Group I was the control and was given normal tap water. Groups II and III received MSG (8 mg/kg) and ASM (32 mg/kg) respectively dissolved in tap water. Group IV received MSG and ASM together in the same doses. After the exposure period, the animals were subjected to cognitive behavioral tests in a shuttle box and a water maze. Thereafter, the animals were sacrificed and the neurotransmitters and oxidative stress indices were estimated in their forebrain tissue. Both MSG and ASM individually as well as in combination had significant disruptive effects on the cognitive responses, memory retention and learning capabilities of the mice in the order (MSG+ASM)>ASM>MSG. Furthermore, while MSG and ASM individually were unable to alter the brain neurotransmitters and the oxidative stress indices, their combination dose (MSG+ASM) decreased significantly the levels of neurotransmitters (dopamine and serotonin) and it also caused oxidative stress by increasing the lipid peroxides measured in the form of thiobarbituric acid-reactive substances (TBARS) and decreasing the level of total glutathione (GSH). Further studies are required to evaluate the synergistic effects of MSG and ASM on the neurotransmitters and oxidative stress indices and their involvement in cognitive dysfunctions.
February 17, 2024
Increased depression, irritabillity and lower cognition among college students consuming artificial sugar aspartame
Professor of Nursing Dept, Univ of North Dakota
Source: Research in Nursing Health, Jun 2014
ABSTRACT
Despite its widespread use, the artificial sweetener aspartame remains one of the most controversial food additives, due to mixed evidence on its neurobehavioral effects. Healthy adults who consumed a study-prepared high-aspartame diet (25 mg/kg body weight/day) for 8 days and a low-aspartame diet (10 mg/kg body weight/day) for 8 days, with a 2-week washout between the diets, were examined for within-subject differences in cognition, depression, mood, and headache. Measures included weight of foods consumed containing aspartame, mood and depression scales, and cognitive tests for working memory and spatial orientation. When consuming high-aspartame diets, participants had more irritable mood, exhibited more depression, and performed worse on spatial orientation tests. Aspartame consumption did not influence working memory. Given that the higher intake level tested here was well below the maximum acceptable daily intake level of 40–50 mg/kg body weight/day, careful consideration is warranted when consuming food products that may affect neurobehavioral health.
February 14, 2024
Environmental exposures & depression
School of Population & Pub Health, Univ of British Columbina, Canada
Source: Annual Reviews in Public Health, Apr 2019
The section entitled "Bisphenol-A and Phthalates" references studies finding reduced BDNF in test animals. BDNF is an essential brain chemical needed for proper brain function, neurogeneis and found low in those with depression. The section entitled "Pesticides" reviews several studies finding they interfere and degrade serotonin and dopamine systems. In fact, two studies are listed finding exposure to pesticides increased the risk of depression. Heavy metals are also explored including cadminum, lead and mercury, all believed to contribute to either blood brain barrier damage, oxidative stress and/or brain cell death. As exposure to all of these factors can be quickly reduced in the person's home and life, it suggests a common-sense first strategy for treating and reducing depression.
..........................................................
ABSTRACT
Mental health and well-being are consistently influenced—directly or indirectly—by multiple environmental exposures. In this review, we have attempted to address some of the most common exposures of the biophysical environment, with a goal of demonstrating how those factors interact with central structures and functions of the brain and thus influence the neurobiology of depression. We emphasize biochemical mechanisms, observational evidence, and areas for future research. Finally, we include aspects of contextual environments—city living, nature, natural disasters, and climate change—and call for improved integration of environmental issues in public health science, policies, and activities. This integration is necessary for reducing the global pandemic of depression.
February 14, 2024
Environmental exposures that damage the brain - Review
Inter Program in Neuroscience, Georgetown University, Washington DC
Source: Environmental Toxicology Pharmacology, May 2021
Here are a few main points brought out by the study authors.
.... perturbation of astrocytic function has far-reaching consequences. This is partly due to the relative abundance of astrocytes compared to other brain cells (Han et al., 2013) and their proximity both to synapses (Agulhon et al., 2008; Allen and Eroglu, 2017) and the blood-brain barrier (Kacem et al., 1998) where they comprise the first line of defense against xenobiotic penetrance of the CNS (Dringen and Hirrlinger, 2003).
.........................................................
ABSTRACT
Exposure to environmental toxicants is linked to long-term adverse outcomes in the brain and involves the dysfunction of glial and neuronal cells. Astrocytes, the most numerous cell type, are increasingly implicated in the pathogenesis of many diseases of the central nervous system, including neurodegenerative diseases. Astrocytes are critical for proper brain function in part due to their robust antioxidant and unique metabolic capabilities. Additionally, astrocytes are positioned both at the blood-brain barrier, where they are the primary responders to xenobiotic penetrance of the CNS, and at synapses where they are in close contact with neurons and synaptic machinery. While exposure to several classes of environmental toxicants, including chlorinated and fluorinated compounds, and trace metals, have been implicated in neurodegenerative diseases, their impact on astrocytes represents an important and growing field of research. Here, we review existing literature focused on the impact of a range of synthetic compounds on astrocytic function. We focus specifically on perturbed metabolic processes in response to these compounds and consider how perturbation of these pathways impacts disease pathogenesis.
February 12, 2024
Antibiotic use increases depression in elderly
School of Public Health, Anhui Medical Univ, China
Source: Environmental Sci Pollution Research Int, Jun 2021
Azithromycin: 81% higher risk of depression
Tetracyclines: 48% higer risk of depression
Veterinary antibiotics: 53% higher risk of depression
When higher levels of antibiotics were given, the risk of depression from tetracyclines more than doubled to 124% for women. In conclusion, the researchers stated, "Our findings reveal that azithromycin, sulfaclozine, tetracyclines, and the VAs were significantly associated with elevated risks of depression in the elderly."
To understand HOW antibiotics increase depression 'Read More..." below.
ANTIBIOICS HARM BODY & BRAIN DEFENSES
The function of antibioitics is to kill bacteria throughout the body. While antibiotics have been in use for over 70 years, it's only been within the past 5-10 years that beneficial bacteria in the human gut have been identified as essential many aspects of human health. This now includes proper immune function - the manufacture of B and D vitamins - production of compounds that improve gut barrier integrity (preventing leaky gut) - blood brain barrier function - and compounds such as butyrate that suppress inflammation. Therefore, any situation that weakens these processes, including antibiotics, would be expected to increase neurological illness such as depression and others.
.........................................................
ABSTRACT
Objective: To examine the associations between urinary antibiotics from various sources and depression in the elderly using the biomonitoring method.
Methods: In the current study, we investigated 990 elderly individuals (≥ 60 years old) from a community-based elderly cohort in West Anhui, China. The participants were interviewed by the Geriatric Depression Scale and self-developed questionnaires. A total of 45 antibiotics belonging to nine categories were screened in urine samples by the developed liquid chromatography electrospray tandem mass spectrometry method. Creatinine-corrected concentrations of antibiotics in urines were used to assess their exposure. Logistic regression analysis was employed to test the relationships between exposure to antibiotics and depression.
Results: Compared to the control group, the multinomial logistic regression analyses showed the elderly exposed to higher concentrations of azithromycin (OR = 1.81, 95% CI: 1.09-3.00) and sulfaclozine (OR = 1.54, 95% CI: 1.05-2.28) had increased risks of depression, respectively. After categorizing the detected antibiotics, tetracyclines (OR = 1.48, 95% CI: 1.02-2.16) and veterinary antibiotics (VAs) (OR = 1.53, 95% CI: 1.06-2.20) were positively correlated with increased risks of depression. After stratified by sex, the VAs (OR = 2.04, 95% CI: 1.13-3.71) at higher concentrations were associated with elevated risks of depression in males, while the associations between depression and antibiotic exposures were observed in tetracyclines (OR = 1.74, 95% CI: 1.04-2.85) and all antibiotics (OR = 2.24, 95% CI: 1.01-2.94) at higher levels in females, respectively. Notably, after the stratification by age, the significant associations were mainly present in the subjects under the age of 70.
Conclusions: Our findings reveal that azithromycin, sulfaclozine, tetracyclines, and the VAs were significantly associated with elevated risks of depression in the elderly. Importantly, sex- and age-specific differences were observed in the associations between antibiotic exposures and depression.
February 12, 2024
Single dose of antibiotics increases risk of depression
Dept of Psychiatry, University College Cork, Ireland
Source: Journal Internal Medicine, Dec 2022
Antibiotics are designed to kill bacteria inside the human body. However, recent discoveries have dramatically changed the way scientists view antibiotic use. For example, trillions of beneficial bacteria in our small and large intestine (gut microbiome) are now understood to be essential for our health - regulating immune system function, reducing autoimmunity, inflammation and increasing serotonin production. In other words, when these beneficial bacteria are destroyed after an antibiotic treatment, they will not be present to perform these critically important brain and body functions. Authors mentioned that the neurotransmitter GABA is produced from gut bacteria known as lactobacilli, but recent studies have shown lactobacilli are reduced by antibiotics, which then resulted in lower GABA production.
Even more concerning, the authors stated, "There is now unequivocal evidence that babies exposed to antibiotics in the first year of life are far more likely to grow up as obese adults and in childhood, are more likely to suffer from asthma, allergies and attention deficit hyperactivity disorder [53]. Both obesity and attention deficit hyperactivity disorder are thought to be mediated by the brain–gut–microbiota axis."
The first report of antibiotic‐induced depression was published as recently as 2010 [54]. A 75‐year‐old man without a history of psychiatric illness became acutely depressed and subsequently committed suicide. He had received antibiotic treatment for a postoperative wound infection following colorectal cancer surgery. The treatment consisted of levofloxacin and trimethoprim sulphamethoxazole and this was considered the principal cause of his suicide at the coroner's court.
...........................................................
ABSTRACT
Antibiotics are recognised as, on occasion, producing psychiatric side effects, most notably depression and anxiety. Apart from antimicrobial activity, antibiotics have multiple off-target effects. The brain-gut-microbiota axis has multiple sites for off-target activity, which may produce either positive or negative antibiotic effects. Here we review how antibiotics impact mental health by acting through the brain-gut-microbiota axis. Microbes in the gut influence brain function by acting through the vagus nerve or by altering the production of short-chain fatty acids or the amino acid tryptophan, the building block of serotonin. Not all antimicrobial actions of antibiotics have a negative impact. The first antidepressant discovered was actually an antibiotic: isoniazid is an antibacterial drug developed for treating tuberculosis. Minocycline, which enters the brain and mediates its effects through microglia, shows antidepressant activity. Some antibiotics bring about a significant decrease in gut microbial diversity, and this is viewed as a risk factor for depression. Other risk factors induced by antibiotics include altered gut barrier function, activation of the hypothalamic-pituitary-adrenal axis, reducing levels of brain-derived neurotrophic factor or oxytocin and alteration of vagal tone. Although most patients taking antibiotics do not suffer from an iatrogenic psychiatric disorder, some do. As clinicians, we need to keep this in mind. The development of new antibiotics is primarily focused on antibiotic resistance, but efforts should be made to reduce off-target brain-gut-microbiota effects resulting in mental health problems.
February 11, 2024
Glyphosate pesticide increases severe depression
Dept of Nephrology, Chang Gung Univ, Taiwan
Source: Environmental Research, Nov 2023
ABSTRACT
Glyphosate, the most widely used herbicide globally, has been linked to neurological impairments in some occupational studies. However, the potential neurotoxic effects of glyphosate exposure in the general population are still not fully understood. We conducted analyses on existing data collected from 1532 adults of the 2013-2014 National Health and Nutrition Examination Survey (NHANES) to explore the possible relationship between glyphosate exposure and cognitive function, depressive symptoms, disability, and neurological medical conditions. Our results showed a significant negative association between urinary glyphosate levels and the Consortium to Establish a Registry for Alzheimer's Disease Word List Memory Test (CERAD-WLT) trial 3 recall and delayed recall scores in both models, with ß coefficients of -0.288 (S.E. = 0.111, P = 0.021) and -0.426 (S.E. = 0.148, P = 0.011), respectively. Furthermore, the odds ratio did not show a significant increase with the severity of depressive symptoms with a one-unit increase in ln-glyphosate levels. However, the odds ratio for severe depressive symptoms was significantly higher than for no symptoms (odds ratio = 4.148 (95% CI = 1.009-17.133), P = 0.049). Notably, the odds ratio showed a significant increase for individuals with serious hearing difficulty (odds ratio = 1.354 (95% CI = 1.018-1.800), P = 0.039) with a one-unit increase in ln-glyphosate levels, but not for other neurological medical conditions. In conclusion, our findings provide the first evidence that glyphosate exposure may be associated with neurological health outcomes in the US adult population. Additional investigation is necessary to understand the potential mechanisms and clinical significance of these correlations.
February 11, 2024
Termite pesticide in homes increases depression - anger - fatigue
Environ Sciences Lab, Univ of S. California School of Medicine
Source: Environmental. Health Perspectives, Jul-Aug 1995
In one instance, 250 adults and children were exposed to chlordane when the wooden building surfaces of their apartment complex was sprayed with chlordane in 1987. In the following years, residents.living in the apartment reported worsening health problems. In June through September of 1994 (7 years after the incident), 216 adults were tested for various neurological effects including depression. Results were as follows when being compared to similar groups not exposed:
Reaction time 34% slower
Memory recall 20% less.
Digit symbol tests 19% lower
Vocabulary score 12% slower
Tension scores 70% higher
Depression state scores 74% worse
Unfortunately, chlordane still outgasses into the air of homes today for homes built prior to 1990. Residents would of course be unaware if this was an issue, but if family members feel better. hours after leaving the home, it should most likely be tested.
............................................................
ABSTRACT
Over 250 adults and children were exposed to chlordane when the wooden building surfaces and soil around an apartment complex were sprayed in 1987. Two hundred-sixteen adults had neurobehavioral functions measured and completed questionnaires for symptom frequency, mood status, confounding factors, and medical, rheumatic, and respiratory disorders in 1994. Measurements included simple and choice reaction time, balance, blink reflex latency, color vision, cognitive, perceptual motor, memory, and recall functions. We analyzed 216 exposed and 174 referent adults. Age, educational level, weight, height, and gender ratio were similar for the exposed and referent groups. Performance of balance, reaction times, Culture Fair, digit symbol, verbal recall, and trail-making were significantly impaired in exposed persons compared to referents. Mood-state scores were elevated, as were the frequencies of respiratory, neurobehavioral, and rheumatic symptoms. In contrast, long-term memory function was similar in both groups, consistent with its status before exposure. There was no identified bias or confounding factors. Chlordane exposure was associated with protracted impairment of neurophysiological and psychological functions. The central nervous system is the most important target of chlorinated cyclodiene insecticides. Human exposure should be prohibited.
February 10, 2024
Monosodium Glutamate (MSG) creates depressive/anxiety behaviors in rats
Federal University of Santa Maria, Brazil
Source: Life Sciences, Jun 2014
The MSG treated animals also showed increased time where no movement was shown in the forced swimming test as well as increased "freezing" reaction in contextual fear conditioning. Additionally, MSG treatment animals had a deregulation of what is called HPA axis function (by increasing serum ACTH and corticosterone levels). In conclusion, the scientists stated, "MSG rats are amore susceptible to develop anxiogenic (anxiety-like) and depressive-like behaviors, which could be related to a dysfunction in the serotonergic system."
...........................................................
ABSTRACT
Monosodium glutamate (MSG) has been the target of research due to its toxicological effects.
Aims: We investigated the depressive- and anxiogenic-like behaviors in rats exposed to neonatal subcutaneous injection of MSG. The involvement of the serotonergic system, by measuring [(3)H] serotonin (5-HT) uptake in cerebral cortices, and the hypothalamic pituitary adrenal (HPA) axis, by determining serum adrenocorticotropic hormone (ACTH) and corticosterone levels, was also examined.
Materials and methods: Male and female newborn Wistar rats were divided into control and MSG groups, which received, respectively, a daily subcutaneous injection of saline (0.9%) or MSG (4 g/kg/day) from the 1st to 5th postnatal day. The behavioral tests [spontaneous locomotor activity, contextual fear conditioning, and forced swimming test (FST)] were performed from the 60th to 64th postnatal day. MSG-treated animals showed alteration in the spontaneous locomotor activity, an increase in the number of fecal pellets and the number of animal's vocalizations and urine occurrence, and a decrease in the grooming time.
Key findings: The MSG exposure increased the immobility time in the FST and the freezing reaction in the contextual fear conditioning. Additionally, MSG treatment increased the [(3)H]5-HT uptake in the cerebral cortices of rats and induced a deregulation of HPA axis function (by increasing serum ACTH and corticosterone levels).
Significance: In conclusion MSG-treated rats are more susceptible to develop anxiogenic- and depressive-like behaviors, which could be related to a dysfunction in the serotonergic system.
February 9, 2024
Phthalate chemical 50-times higher in depressed women
Dept of Pharmacology, Natl Autonomous Univ of Mexico
Source: Int J Environ Research & Public Health, Feb 2022
All subjects were tested for 4 different Phthalates and 2 Bisphenols (BPA and BPS). While no significant differences were found in BPA and BPS between the groups, the level of one phthalate was dramatically higher in women. The chemical, butyl-benzyl-phthalate (BBP), was found 50 times higher in depressed women compared to depressed men.
It's interesting to note that women in the general population have higher levels of phthalates in their blood than men. An explanation for this is women use more products that contain phthalates, such as cosmetics. Also of interest, researchers cited a study showing BBP was found to cause a decrease in serotonin im test animals (71). It is also reported to increase oxidative damage to cells. The chemical also crosses the placental barrier suggesting harm may begin as early as pregnancy, thereby predisposing the idividual to depression and other neurological disorders at a later date.
In their concluding paragraph, the researchers stated, "Our results suggested that phthalate exposure, particularly BBP, might increase MDD in female adults. However, our findings warrant further studies in larger population. This study lays the foundations for making associations between exposure to EDCs and the development of MDD since there is insufficient evidence on this aspect."
.........................................................
ABSTRACT
Public concern has emerged about the effects of endocrine-disrupting compounds (EDCs) on neuropsychiatric disorders. Preclinical evidence suggests that exposure to EDCs is associated with the development of major depressive disorder (MDD) and could result in neural degeneration. The interaction of EDCs with hormonal receptors is the best-described mechanism of their biological activity. However, the dysregulation of the hypothalamic-pituitary-gonadal adrenal axis has been reported and linked to neurological disorders. At a worldwide level and in Mexico, the incidence of MDD has recently been increasing. Of note, in Mexico, there are no clinical associations on blood levels of EDCs and the incidence of the MDD. Methodology: Thus, we quantified for the first time the serum levels of parent compounds of two bisphenols and four phthalates in patients with MDD. The levels of di-ethyl-hexyl-phthalate (DEHP), butyl-benzyl-phthalate (BBP), di-n-butyl phthalate (DBP), and di-ethyl-phthalate (DEP), bisphenol A (BPA), and bisphenol S (BPS) in men and women with or without MDD were determined with a gas chromatograph-mass spectrometer. Results/conclusion: We found significant differences between concentrations of BBP between controls and patients with MDD. Interestingly, the serum levels of this compound have a dysmorphic behavior, being much higher in women (~500 ng/mL) than in men (≤10 ng/mL). We did not observe significant changes in the serum concentrations of the other phthalates or bisphenols tested, neither when comparing healthy and sick subjects nor when they were compared by gender. The results point out that BBP has a critical impact on the etiology of MDD disorder in Mexican patients, specifically in women.
February 9, 2024
Defective Blood Brain Barrier as cause of depression
Dept of Psychiatry, University of Miami, FL
Source: Neurobiology of Disease, Nov 2022
Interestingly, a number of environmental factors have recently been identified that either directly cause neuroinflammation or blood brain barrier defects. For example, in a post in our "Causes" section, we discuss studies showing a common chemical known as Phthaltes can disrupt the BBB at normal and low environmental doses. The biggest sources of phthalate exposure for humans includes vinyl flooring, fragrances such as plug-in air fresheners and perfumes, cosmetics, nail polishes and plastic storage containers which leach into and concentrate in food. With the documentation that phthalates disrupt the BBB at levels. commonly found in homes and the environment, it would suggest immediate efforts should be made to remove these sources.
......................................................
ABSTRACT
The blood brain barrier (BBB) is a vital structure to protect the brain, tightly filtering the passage of nutrients and molecules from the blood to the brain. This is critical for maintaining the proper functioning of the brain, and any disruption in the BBB has detrimental consequences often leading to diseases. It is not clear whether disruption of the BBB occurs first in depression or is the consequence of the disease, however disruption of the BBB has been observed in depressed patients and evidence points to the role of important culprits in depression, stress and inflammation in disrupting the integrity of the BBB. The mechanisms whereby stress, and inflammation affect the BBB remain to be fully understood. Yet, the role of cytokines in regulating tight junction protein expression seems crucial. Altogether, the findings in depression suggest that acting at the BBB level might provide therapeutic benefit in depression.
February 7, 2024
The metal cadmium (used in chemical fertilizers) increases depression 21%
Dept of Pharmacy, Sunchon National Univ, S. Korea
Source: Environ Science Pollution Research, Jan 2022
While no significant differences in lead or mercury were found between those with or without depression, those with depression were found to have significantly higher levels of cadmium. In fact, each "doubling" of cadmium level resulted in a 21% increase in depression. Therefore, having a 4-fold higher level of cadmium would result in a 42% higher risk of depression. This strongly suggests that switching to organically grown food (which would reduce cadmium levels about 50%) should be one of the first strategies implemented for treating depression. Bringing more interest to the topic, researchers at Newcastle University in the UK found organically grown food (which uses natural fertilizers) had 48% less cadmium. The World Health Orgnaization (WHO) stated in 2021 that depressed patients are frequently not correctly diagnosed, and others who do not have a depressive disorder are too frequently misdiagnosed and prescribed antidepressants. This would stress the importance of considering environmental factors as a cause of depression BEFORE initiating pharmaceutical drug treaments. To view the 2014 study showing 48% lower cadmium in organically grown food - copy and paste the following link.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4141693/
.............................................
ABSTRACT
Little is known about associations between depression and serum heavy metal levels, dietary vitamin intakes. Thus, we sought to determine the nature of these associations and to predict risks of depression using marginal effects. A data set of 16,371 individuals aged ≥10 years that participated in Korea National Health and Nutrition Examination Surveys (KNHANES) conducted from 2009 to 2017 (excluding 2014 and 2015) was used to obtain information on sociodemographics, family histories, lifestyles, serum heavy metal levels, food intakes, and depression. Serum cadmium (Cd) and lead (Pb) levels were analyzed by graphite furnace atomic absorption spectrometry and mercury (Hg) levels using a mercury analyzer. Daily vitamin intakes were calculated by 24-h dietary recall. The results obtained showed that females are at higher risk of depression than males. A doubling of serum Cd was associated with a 21% increase in depression (AOR 1.21, 95% CI: 1.07–1.37, p = 0.002), whereas twofold increases in daily vitamin B1, B3 and vitamin A intakes reduced the risk of depression by 17% (0.83, 95% CI: 0.73–0.95, p = 0.005), 20% (0.80, 95% CI: 0.70–0.91, p = 0.001), and 8% (0.92, 95% CI: 0.85–0.99, p = 0.020), respectively. Interactions between heavy metals, vitamin intakes, and sex did not influence the risk of depression. The result shows that increased daily dietary vitamin intake might protect the public against depression. Further studies are needed to reduce the risks posed by heavy metals and to determine more comprehensively the effects of daily dietary vitamin intake on depression.
February 5, 2024
Poor diet strongly linked to Depressive Disorder
Dept of Nutrition, Ankara Medical Univ, Turkey
Source: Experimental Gerontology, Feb 2023
ABSTRACT
Depression is one of the leading health problems, and >300 million people have a major depressive disorder and this number is getting increasing. Depression complicates the management of existing chronic diseases and the management of complications that may arise. A person's mental state can affect their food preferences, and food preferences can also affect their mental state. In this paper, depression and eating behavior, diet quality, folic acid, vitamin B12, vitamin B6, vitamin D, omega-3 fatty acids, magnesium, selenium, zinc and copper, prebiotics and probiotics are discussed. Research on the subject emphasizes that diet quality may also affect the occurrence of depression. However, studies also indicated that dietary nutrients such as folic acid, vitamin B12, vitamin B6, omega-3 fatty acids, zinc, selenium, and magnesium might be associated with the risk of depression.
February 2, 2024
Urine samples show pesticides increase depression
Anhui Medical University, China
Source: Environmental Pollution, Jan 2023
ABSTRACT
Organophosphorus pesticides (OPPs) are widely used pesticides, and previous studies showed that OPPs can increase the risk of central nervous system disorders (e.g., Parkinson's and Alzheimer's disease). However, few studies have comprehensively explored their association with depression in general adults. We analyzed data from 5206 participants aged 20 years or more based on four National Health and Nutrition Examination Survey (NHANES) cycles. OPPs exposure was estimated using measures of urinary concentrations for six OPPs metabolites. Survey-weighted generalized linear regression model (SWGLM) was used to explore the association of OPPs metabolites with depression. Subgroup analyses were performed by age (≦60 years and >60 years) and gender. The weighted quantile sum (WQS) regression model was used to explore the overall association of six OPPs metabolites with depression. In addition, The Bayesian kernel machine regression (BKMR) model was applied to investigate the interaction and joint effects of multiple OPPs metabolites with depression. The SWGLM showed that dimethyl phosphate (DMP) and dimethyl thiophosphate (DMTP), whether taken as continuous or quartile variables, had a positive correlation with depression. Diethyl phosphate (DEP) and dimethyl dithiophosphate (DMDTP) in the highest quartile were positively associated with depression compared to the lowest quartile. In subgroup analysis, we found that the effects of the above chemicals on depression existed in the male and young middle-aged population, while DMP was present in the female. There was a significant combined overall effect of six OPPs metabolites with depression [OR = 1.232, 95%CI: (1.011, 1.504)] in WQS. Furthermore, the BKMR model also showed a positive trend in the overall effect of six OPPs metabolites with depression. In conclusion, our results suggest that exposure to OPPs may increase the risk of depression in US adults. Men and young and middle-aged populations are more vulnerable to OPPs and the mixture of OPPs metabolites may induce depression.
January 25, 2024
Mercury from silver fillings linked to excessive anger, depression, and anxiety
Rocky Mtn Research Institute, Fort Collins, CO
Source: Psychological Reports, Feb 1994
ABSTRACTScores on the Beck Depression Inventory were compared for 25 women who had silver dental fillings (amalgams) and for 23 women without amalgams. Women with amalgams had significantly higher scores and reported more symptoms of fatigue and insomnia. Anger scores from the State-Trait Anger Expression Inventory showed that the women with amalgams had statistically significantly higher mean scores on expressing anger without provocation and experiencing more intense angry feelings. The women without amalgams scored significantly higher on controlling anger, which suggested they invested more energy in monitoring and preventing the experience and expression of anger. Anxiety scores from the State-Trait Anxiety Inventory showed the women with amalgams scored significantly less pleasant, satisfied, happy, secure, and steady, and had a more difficult time making decisions. They had significantly higher Trait Anxiety scores. The women with amalgams also had significantly higher levels of mercury in the oral cavity before and after chewing gum. The study suggests that amalgam mercury may be an etiological factor in depression, excessive anger, and anxiety because mercury can produce such symptoms perhaps by affecting the neurotransmitters in the brain.
January 22, 2024
Home pesticide use increases depression
Guangzhou Ctr for Disease Control & Prevention, China
Source: Environmental Research, Sep 2020
Background: The effect of household pesticide exposure on depressive symptoms in the general population is underexplored, and the role of exercise in the association between pesticide exposure and depressive symptoms is unclear.
Objective: The goals of this study are to examine whether the associations between household pesticide exposure and depressive symptoms exist in the general population, and whether exercise can attenuate these associations.
Methods: We used data from the 2005-2014 National Health and Nutrition Examination Surveys (NHANES), including a total of 14708 US adult participants who were 20 years or older. Depressive symptoms were assessed using the Patient Health Questionnaire (PHQ-9). Exercise information on the recreational physical activity (RPA) and pesticide exposure were self-reported in an interview.
Results: Participants with exposure of household pesticide had a higher odds ratio ([OR]; OR = 1.32, 95% confidence intervals [CI]: 1.12-1.56) for depressive symptoms, compared to those who had not been unexposed. A significant interaction between exercise and pesticide exposure on depressive symptoms was observed (P = 0.038). Stratified analysis showed that household pesticide exposure was associated with a 50% higher risk of depressive symptoms (OR = 1.50, 95% CI: 1.20-1.86) in the population with light RPA. However, we did not find a significant association in the group with moderate + vigorous RPA (P = 0.305).
Conclusion: This study further confirms that household pesticide exposure is associated with an elevated risk of depressive symptoms in the general population. More importantly, we for the first time reports that moderate + vigorous RPA attenuates the positive association between household pesticide exposure and depressive symptoms.
January 4, 2024
Dental mercury fillings suspected of increasing depression
Institute of Chronic Illness, Silver Sp, MD
Source: Neurological Endocrinology Letters, 1994
ABSTRACT
The purpose of this review is to examine the evidence for a relationship between mercury (Hg) exposure from dental amalgams and certain idiopathic chronic illnesses--chronic fatigue syndrome (CFS), fibromyalgia (FM), depression, anxiety, and suicide. Dental amalgam is a commonly used dental restorative material that contains approximately 50% elemental mercury (Hg0) by weight and releases Hg0 vapor. Studies have shown that chronic Hg exposure from various sources including dental amalgams is associated with numerous health complaints, including fatigue, anxiety, and depression--and these are among the main symptoms that are associated with CFS and FM. In addition, several studies have shown that the removal of amalgams is associated with improvement in these symptoms. Although the issue of amalgam safety is still under debate, the preponderance of evidence suggests that Hg exposure from dental amalgams may cause or contribute to many chronic conditions. Thus, consideration of Hg toxicity may be central to the effective clinical investigation of many chronic illnesses, particularly those involving fatigue and depression.
April 21, 2023
Higher PFAS = Higher Depression in pregnant women
University of Southern California
Source: Environmental International, Feb 2023
Quartile 2: U.S. born 9% higher depression - Immigrants 12% higher
Quartile 3: U.S. born 18% higher depresison - Immigrants 24% higher
Quartile 4: U.S. born 27% higher depresison - Immigants 36% higher.
More information on common household sources of PFAS are listed in the 'Read More' section below.
PFAS chemicals are added to many products to resist water and oil. Reports have shown PFAS is very common in women's makeup (to resist perspiration)and very high in mascara, lipstick, lotions, sunscreens and also high in fast food wrappers (burgers, fries, etc). It is used in floor products, furniture upholstery, carpet, stain guard chemicals, etc.
Researchers was stated PFAS to increase inflammation which studies strongly agree is a major driver underlying depression. Below is a direct quote from their introduction as seen in the PDF.
"There is increasing evidence that human exposure to PFAS affects several intermediate biological mechanisms, including inflammation, oxidative stress, hormone signaling, and lipid metabolism (Fenton et al., 2021). While PFAS can accumulate in various tissues in the human body, a recent review highlighted evidence from human, animal, and in vitro studies indicating that PFAS can accumulate in the brain and nervous tissue potentially by interfering with tight junctions at the blood brain barrier and interacting with transmembrane transporters (Cao and Ng, 2021)."
.............................................
ABSTRACT
Exposure to per- and poly-fluoroalkyl substances (PFAS) remains an important public health issue due to widespread detection and persistence in environmental media, slow metabolism in humans, and influences on physiological processes such as neurological signaling. Maternal depression is highly prevalent during pregnancy and postpartum and is potentially sensitive to PFAS. The health risks associated with PFAS may be further amplified in historically marginalized communities, including immigrants.
Objective
Evaluate maternal concentrations of PFAS in association with depression scores during pregnancy and whether effects differ between US born and immigrant women.
Methods
Our study sample included 282 US born and 235 immigrant pregnant women enrolled in the Chemicals in Our Bodies prospective birth cohort based in San Francisco, CA. We measured 12 PFAS in serum samples collected in the second trimester and depressive symptom scores were assessed using the Center for Epidemiologic Studies Depression Scale. Associations were estimated using linear regression, adjusting for maternal age, education, pre-pregnancy body mass index, and parity. Associations with a PFAS mixture were estimated using quantile g-computation.
Results
In adjusted linear regression models, a twofold increase in two PFAS was associated with higher depression scores in the overall sample, and this association persisted only among immigrant women (β [95 % confidence interval]: perfluorooctane sulfonic acid (2.7 [0.7–4.7]) and methyl-perfluorooctane sulfonamide acetic acid (2.9 [1.2–4.7]). Quantile g-computation indicated that simultaneously increasing all PFAS in the mixture by one quartile was associated with increased depressive symptoms among immigrant women (mean change per quartile increase = 1.12 [0.002, 2.3]), and associations were stronger compared to US born women (mean change per quartile increase = 0.09 [-1.0, 0.8]).
Conclusions
Findings provide new evidence that PFAS are associated with higher depression symptoms among immigrant women during pregnancy. Results can inform efforts to address environmental factors that may affect depression among US immigrants.
December 6, 2022
Amphetamines cause neuroinflammation - worsening depression
Univ do Porto, Portugal, Addiction Biology
Source: Frontiers Cell Neuroscience, May 2023
ABSTRACT
It is now well-accepted that psychostimulants act on glial cells causing neuroinflammation and adding to the neurotoxic effects of such substances. Neuroinflammation can be described as an inflammatory response, within the CNS, mediated through several cytokines, reactive oxygen species, chemokines and other inflammatory markers. These inflammatory players, in particular cytokines, play important roles. Several studies have demonstrated that psychostimulants impact on cytokine production and release, both centrally and at the peripheral level. Nevertheless, the available data is often contradictory. Because understanding how cytokines are modulated by psychoactive substances seems crucial to perspective successful therapeutic interventions, here, we conducted a scoping review of the available literature. We have focused on how different psychostimulants impact on the cytokine profile. Publications were grouped according to the substance addressed (methamphetamine, cocaine, methylphenidate, MDMA or other amphetamines), the type of exposure and period of evaluation (acute, short- or long-term exposure, withdrawal, and reinstatement). Studies were further divided in those addressing central cytokines, circulating (peripheral) levels, or both. Our analysis showed that the classical pro-inflammatory cytokines TNF-α, IL-6, and IL-1β were those more investigated. The majority of studies have reported increased levels of these cytokines in the central nervous system after acute or repeated drug. However, studies investigating cytokine levels during withdrawal or reinstatement have shown higher variability in their findings. Although we have identified fewer studies addressing circulating cytokines in humans, the available data suggest that the results may be more robust in animal models than in patients with problematic drug use. As a major conclusion, an extensive use of arrays for relevant cytokines should be considered to better determine which cytokines, upon the classical ones, may be involved in the progression from episodic use to the development of addiction. A concerted effort is still necessary to address the link between peripheral and central immune players, including from a longitudinal perspective. Until there, the identification of new biomarkers and therapeutic targets to envision personalized immune-based therapeutics will continue to be unlikely.
The percentage of people with depression has increased dramatically since the 1960s. Numbers in the U.S, Australia and several other industrialized countries are increasing even faster. While stabilizing somewhat in adults over 50, depression rates among children and young adults are rising at an unprecedented rate causing extreme concern among public health officials. Rapidly rising rates suggest environmental rather than genetic factors are involved. Here we look at various studies investigating the numbers behind depression.
February 10, 2024
Depression rising dramatically in U.S. children 2015-2020
Graduate School of Pub Health and Health Policy, City Univ of NY
Source: American Journal of Preventive Medicine, Nov 2022
The biggest concern, that should frighten all of us frankly, is how fast these rates are rising. Looking at the 12-17 aged group, depression went from 12.7% in 2015 to 16.9% in 2020, so a 33% increase in 5 years.
For those aged 18-25, depression was only 10.3% in 2015 and then jumped to 17.2% in 2020. So, a much larger rise here, up nearly 70% in 5 short years. Interestingly, no increases were seen in adults aged 35-49 or over 50 years of age.
Depression was also nearly twice as common in women than men with caucasian women being the group most affected. The numbers reported here are all from the United States, but apparently, other countries are seeing massive increases in depression in children and young adults as well. In another 2023 study from Australia (also reviewed in this section), the rates of depression for children aged 10-24 was 21.3%. When anxiety was included with depression, the rate jumped to 29.9%.
Certainly, when a form of mental illness is rising with such ferocity in our youngest population (who will soon be in charge of our future), it's important to identify WHY this is happening. When changes happen quickly over such a short period of time, genetics or psychological explanations are obviously not the primary factor, which leads us to something we are eating, drinking, breathing or doing as the reason for the rapid rise. In other words - environmental factors. With many abnormalities now depression now shown to result from many abnormalities inside the human body (including inflammation, gut abnormalities, blood brain bvarrier break-down). If we are willing to address and acknowledge our mistakes, that's the real question.
.........................................................
ABSTRACT
Introduction
Major depression is a common and potentially lethal condition. Early data suggest that the population-level burden of depression has been exacerbated by the COVID-19 pandemic. Prepandemic estimates of depression prevalence are required to quantify and comprehensively address the pandemic's impact on mental health in the U.S.
Methods
Data were drawn from the 2015–2020 National Survey on Drug Use and Health, a nationally representative study of U.S. individuals aged ≥12 years. The prevalence of past-year depression and help seeking for depression were estimated from 2015 to 2019, and time trends were tested with Poisson regression with robust SEs. Point estimates were calculated for 2020 and not included in statistical trend analyses because of differences in data collection procedures.
Results
In 2020, 9.2% (SE=0.31) of Americans aged ≥12 years experienced a past-year major depressive episode. Depression was more common among young adults aged 18–25 years (17.2%, SE=0.78), followed closely by adolescents aged 12–17 years (16.9%, SE=0.84). Depression increased most rapidly among adolescents and young adults and increased among nearly all sex, racial/ethnic, income, and education groups. Depression prevalence did not change among adults aged ≥35 years, and the prevalence of help seeking remained consistently low across the study period.
Conclusions
From 2015 to 2019, there were widespread increases in depression without commensurate increases in treatment, and in 2020, past 12‒month depression was prevalent among nearly 1 in 10 Americans and almost 1 in 5 adolescents and young adults. Decisive action involving a multipronged public health campaign that includes evidence-based prevention and intervention to address this ongoing mental health crisis is urgently needed.
February 8, 2024
Depression numbers in 1996
Dept of Psychiatry, Columbia University, NY
Source: JAMA, July 1996
Unfortunately, these are the only numbers available from the Abstract. At a future date, I will get hold of the full-version to post depression numbers for other countries. We can then compare numbers here (which are mostly from the early 1990s and 1980s) to numbers today.
...........................................................
ABSTRACT
Objective: To estimate the rates and patterns of major depression and bipolar disorder based on cross-national epidemiologic surveys.
Design and setting: Population-based epidemiologic studies using similar methods from 10 countries: the United States, Canada, Puerto Rico, France, West Germany, Italy, Lebanon, Taiwan, Korea, and New Zealand.
Participants: Approximately 38000 community subjects.
Outcome measures: Rates, demographics, and age at onset of major depression and bipolar disorder. Symptom profiles, comorbidity, and marital status with major depression.
Results: The lifetime rates for major depression vary widely across countries, ranging from 1.5 cases per 100 adults in the sample in Taiwan to 19.0 cases per 100 adults in Beirut. The annual rates ranged from 0.8 cases per 100 adults in Taiwan to 5.8 cases per 100 adults in New Zealand. The mean age at onset shows less variation (range, 24.8-34.8 years). In every country, the rates of major depression were higher for women than men. By contrast, the lifetime rates of bipolar disorder are more consistent across countries (0.3/100 in Taiwan to 1.5/100 in New Zealand); the sex ratios are nearly equal; and the age at first onset is earlier (average, 6 years) than the onset of major depression. Insomnia and loss of energy occurred in most persons with major depression at each site. Persons with major depression were also at increased risk for comorbidity with substance abuse and anxiety disorders at all sites. Persons who were separated or divorced had significantly higher rates of major depression than married persons in most of the countries, and the risk was somewhat greater for divorced or separated men than women in most countries.
Conclusions: There are striking similarities across countries in patterns of major depression and of bipolar disorder. The differences in rates for major depression across countries suggest that cultural differences or different risk factors affect the expression of the disorder.
September 1, 2023
Adolescent depression doubles in 10 years - 2009-2019
Dept of Psychology, Maynooth Univ. Ireland
Source: J Adolescent Health, Mar 2022
ABSTRACT
Purpose
Major depression is a leading cause of disability and represents a significant health concern for adolescents. Evidence of temporal trends in adolescent depression stratified by sociodemographic characteristics is needed.
Methods
This study drew on 11 years of the National Survey on Drug Use and Health (N = 167,783), a nationally representative survey of adolescents aged 12–17 years conducted between 2009 and 2019.
Results
The prevalence of past-year major depressive episode (MDE) increased by 7.7 percentage points from 8.1% to 15.8% between 2009 and 2019. MDE increased by 12 percentage points from 11.4% to 23.4% among girls. The gender difference in the prevalence of MDE increased from 6.4% to 14.8% between 2009 and 2019. Black participants experienced a comparatively small increase in depression (4.1%).
Conclusions
Since 2009 there has been a sharp and sustained increase in depression among adolescent girls in the U.S. This concerning trend highlights the critical importance of directing prevention and intervention efforts toward this group.
Rather than begin with phamaceutical medications (which show a low 20-36% effectivness in treating depression), the scientists who study depression are stating other treatment strategies should be tried first. For example, as mentioned repeatedly in the literature, abnormal levels of gut bacteria are found in nearly all patients with depressive disorder. Since gut bacteria manufacture serotonin and essential vitamins, this suggests alterations in diet and food choices should be implemented prior to pharmaceutical interventions. This section discusses a number of non-pharmaceutical treatment strategies that have been shown or would suggest a higher success rate. Emphasis on reducing neuroinflammation is also discussed.
March 17, 2024
Neurological disorders caused by gut bacteria abnormalities - improved by probiotics & dietary fibers
Dept of Exp Psychology, Univ of Seville, Spain
Source: Psychoneuroendocrinology, Mar 2022
Individuals with depression were shown to have higher inflammatory markers which predicted certain psychological factors. The results suggest that Lactoba- cillus and inflammation could be differentially associated with mood disorder through brain mechanisms that support self-judgment and empathy (Heym et al., 2019). Additionally, it was found that different psychobiotics, mainly dietary fibers and probiotics of the Lactobacillus family, improved different cognitive functions such as cognitive performance.
ABSTRACT
The gut microbiota is the set of microorganisms present in the gut, and it is connected to the central nervous system via the gut-brain axis. Despite there is not a definitive description of the eubiotic microbiota architecture, numerous studies have demonstrated its involvement in human behaviour and its relationship with several pathologies. This is a systematic review about the association between dysbiosis on the gut microbiota and the presence of neurological or neuropsychiatric diseases such as cognitive impairment, Alzheimer's disease, Parkinson's disease, ADHD, and depression. Furthermore, this study analyzes the potential benefits of psychobiotics supplementation for these pathologies. Searches were conducted in the electronic databases PubMed and PsycINFO. 17 articles were included in this review, the majority were published after 2019. The results showed that gut dysbiosis predicts the development of these pathologies and influences their pathogenesis. In addition, it was found that different psychobiotics, mainly dietary fibers and probiotics of the Lactobacillus family, improved different cognitive functions such as cognitive performance and induce a reduced cortisol response. Improvement in different cognitive functions is possible when understanding gut microbiota-brain axis, enteric nervous system, neural-immune system, neuroendocrine system, and central nervous system's relationship.
March 7, 2024
Anxiety & Eating Disorders - improved by probiotics
Biomedical Research Institute, Barcelona Spain
Source: Int J Molecular Science, Mar 2021
ABSTRACT
Anxiety and eating disorders produce a physiological imbalance that triggers alterations in the abundance and composition of gut microbiota. Moreover, the gut–brain axis can be altered by several factors such as diet, lifestyle, infections, and antibiotic treatment. Diet alterations generate gut dysbiosis, which affects immune system responses, inflammation mechanisms, the intestinal permeability, as well as the production of short chain fatty acids and neurotransmitters by gut microbiota, which are essential to the correct function of neurological processes.
Recent studies indicated that patients with generalized anxiety or eating disorders (anorexia nervosa, bulimia nervosa, and binge-eating disorders) show a specific profile of gut microbiota, and this imbalance can be partially restored after a single or multi-strain probiotic supplementation. Following the PRISMA methodology, the current review addresses the main microbial signatures observed in patients with generalized anxiety and/or eating disorders as well as the importance of probiotics as a preventive or a therapeutic tool in these pathologies.
February 26, 2024
Exercise reduces both aggression & depression in college students
School of Physical Education, Southwest Univ, China
Source: Psychological Research Behavioral Mngt, Jan 2024
ABSTRACT
Purpose
The deleterious impact of aggressive behavior on college students necessitates urgent mitigation. To explore the influencing factors and underlying mechanisms of aggressive behaviors among college students, this study aims to validate the mediating roles of life satisfaction, meaning in life, and depression by examining the relationship between physical exercise and aggressive behaviors among college students.
Methods
The Physical Activity Rating Scale-3 (PARS-3), Satisfaction with Life Scale, Meaning in Life Questionnaire, Chinese Version DASS-21 and 12-item Perception of Aggression Scale (POAS) were tested on 1596 college students from three universities in western China, and SPSS 26.0 and Mplus 8.3 were used for analysis.
Results
Physical exercise exhibited a significant negative correlation with both aggressive behaviors and depression among college students (r = –0.57, P < 0.001; r = –0.36, P < 0.001), as well as a significant positive correlation with life satisfaction and meaning in life (r = 0.45, P < 0.001; r = 0.27, P < 0.001). Regarding the impact of physical exercise on aggressive behaviors among college students, the mediating effects of life satisfaction, meaning in life, and depression were significant. The respective effect sizes were −0.11, −0.08, and −0.03. The chain mediation effect of life satisfaction through depression was also found to be significant, with an effect size of −0.02.
Conclusion
This study elucidates the mechanistic pathways through which physical exercise influences aggressive behavior among college students. The relationship between physical exercise and aggressive behavior is influenced by the individual mediating effects of life satisfaction, meaning in life, and depression, as well as the chain mediation effect of life satisfaction through depression. These findings provide a novel perspective on the prevention and intervention of aggressive behaviors among college students in China and potentially worldwide. This suggests that more attention should be paid to the organic combination of students’ physical activity and mental health education.
February 26, 2024
Exercise improves mental health in patients with major depression
Dept of Rehabilitation Sciences, Belgium
Source: Disability Rehabilitation, 2015
ABSTRACT
Purpose: to present clinical guidelines for exercise therapy in depressed patients derived from recent meta-analyses.
Method: four meta-analyses on effects of physical exercise on mental and physical in depression were analysed.
Results: For mild to moderate depression the effect of exercise may be comparable to antidepressant medication and psychotherapy; for severe depression exercise seems to be a valuable complementary therapy to the traditional treatments. Depression is associated with a high incidence of co-morbid somatic illnesses, especially cardiovascular diseases, type 2 diabetes and metabolic syndrome. Exercise is extremely powerful in preventing and treating these diseases. Physical exercise is an outstanding opportunity for the treatment of patients who have a mix of mental and physical health problems. Exercise therapy also improves body image, patient s coping strategies with stress, quality of life and independence in activities of daily living in older adults.
Conclusions: Physical therapists should be aware, that several characteristics of major depression (e.g. loss of interest, motivation and energy, generalised fatigue, a low self-worth and self-confidence, fear to move, and psychosomatic complaints) and physical health problems interfere with participation in exercise. Therefore, motivational strategies should be incorporated in exercise interventions to enhance the patients' motivation and adherence in exercise programs. Implications for Rehabilitation For mild to moderate depression, the effect of exercise may be comparable with antidepressant medication and psychotherapy; for severe depression, exercise seems to be a valuable complementary therapy to the traditional treatments. Exercise therapy also improves physical health, body image, patient's coping strategies with stress, quality of life, and independence in activities of daily living in older adults. Motivational strategies should be incorporated in exercise interventions to enhance the patients' motivation.
February 22, 2024
Would stopping alcohol restore blood brain barrier depression defense?
Dept of Psychology, Binghamton Univ-State Univ of NY
Source: International Reveiews Neurobiology, Jun 2022
Alcohol is the most commonly used drug of abuse in the world and binge drinking is especially harmful to the brain, though the mechanisms by which alcohol compromises overall brain health remain somewhat elusive. A number of brain diseases and pathological states are accompanied by perturbations in Blood-Brain Barrier (BBB) function, ultimately exacerbating disease progression. The BBB is critical for coordinating activity between the peripheral immune system and the brain. Importantly, BBB integrity is responsive to circulating cytokines and other immune-related signaling molecules, which are powerfully modulated by alcohol exposure. This review will highlight key cellular components of the BBB; discuss mechanisms by which permeability is achieved; offer insight into methodological approaches for assessing BBB integrity; and forecast how alcohol-induced changes in the peripheral and central immune systems might influence BBB function in individuals with a history of binge drinking and ultimately Alcohol Use Disorders (AUD).
February 18, 2024
Psychological stress damages brain but reversed by plant neutraceutical quercetin
Dept Lab Medicine, A Hosp Yangzhou Univ, China
Source: Molecular Neurobiology, Feb 2024
SOURCES OF QUERCETIN
As this study suggests quercetin can reduce depression by various means, here is a list of foods with the highest levels of quercetin. Number represents milligrams of quercetin per 100 grams of the plant.
1. Capers (raw) - 234 mg
2. Lovage leaves (raw) 170 mg
3. Sorrel - 86 mg
4. Radish leaves - 70 mg
5. Carob fiber - 58 mg
6. Coriander - 53 mg
7. Fennel leaves - 49 mg
8. Red Onion - 32 mg
9. Black Plums - 12 mg
Interestingly, one study in Wikipedia found quercetin was 79% higher in organic tomatoes when compared to non-organic conventionally grown. This advantage may be true with other organic fruits and vegetables as well. While quercetin is availble in pill form, it may be more active and availble in foods.
ABSTRACT
Cognitive dysfunction was a common symptom of major depressive disorder (MDD). In previous studies, psychological stress leads to activation and proliferation of microglial cells in different brain regions. Quercetin, a bioflavonoid derived from vegetables and fruits, exerts anti-inflammatory effects in various diseases. To demonstrate the role of quercetin in the hippocampal inflammatory response in depress mice. The chronic unpredictable stress (CUS) depressive mice model built is used to explore the protective effects of quercetin on depression. Neurobehavioral test, protein expression of NOD-like receptor thermal protein domain associated protein 3 (NLRP3) and heat shock protein 90 (HSP90), and cytokines (IL-6, IL-1β, MCP-1, and TNF-α) were assessed. Quercetin ameliorated depressive-like behavior and cognitive impairment, and quercetin attenuates neuroinflammation and by targeting HSP90 to inhibit NLRP3 inflammasome activation. Quercetin inhibited the increase of HSP90 levels in the hippocampus and reverses inflammation-induced cognitive impairment. Besides, quercetin inhibited the increased level of cytokines (IL-6, IL-1β, MCP-1, and TNF-α) in the hippocampus of the depressive model mouse and the increased level of cytokines (IL-6, IL-1β, and MCP-1) in microglia. The current study indicated that quercetin mitigated depressive-like behavior and by targeting HSP90 to inhibit NLRP3 inflammasome activation in microglia and depressive mice model, meanwhile ameliorated cognitive impairment in depression. Quercetin has huge potential for the novel pharmacological efficacy of antidepressant therapy.
February 13, 2024
High Green Tea consumption in elderly dramatically reduces depression
Div of Biomed Eng Health and Welfare, Tohoku University
Source: Am J Clin Nutrition, Dec 2009
1. Drinking green tea less than or equal to 1 cup/day
2. Drinknig green tea 2-3 cups/day
3. Driking green tea 4 or more cups/day
Groups also included consumption of black tea and coffee. When looking at all 1,058 subjects, those consuming 2-3 cups/day of green tea had a 4% reduction in depression, however, those consuming 4 or more cups of green tea daily had a 46% reduction in depressive symptoms. For their explanation "why" green tea was believed to reduce rates of depression 'Read More..' below.
At first, researchers believed it was the reduction in inflammation from green tea compounds that resulted in its powerful effects for preventing depression. However, further testing showed this did not appear to be the case as C-reaction protein (a marker for general body inflammation) was not different in the different tea consumption groups. Other facts are being hypothesized including its ability to improve the mucin gut barrier as well as increasing serotonine and new brain cell growth (both of which green tea has been shown to do).
.......................................................
ABSTRACT
Background
Green tea is reported to have various beneficial effects (eg, anti–stress response and antiinflammatory effects) on human health. Although these functions might be associated with the development and progression of depressive symptoms, no studies have investigated the relation between green tea consumption and depressive symptoms in a community-dwelling population.
Objective
The aim of this study was to investigate the relations between green tea consumption and depressive symptoms in elderly Japanese subjects who widely consumed green tea.
Design
We conducted a cross-sectional study in 1058 community-dwelling elderly Japanese individuals aged ≥70 y. Green tea consumption was assessed by using a self-administered questionnaire, and depressive symptoms were evaluated by using the 30-item Geriatric Depression Scale with 2 cutoffs: 11 (mild and severe depressive symptoms) and 14 (severe depressive symptoms). If a participant was consuming antidepressants, he or she was considered to have depressive symptoms.
Results
The prevalence of mild and severe and severe depressive symptoms was 34.1% and 20.2%, respectively. After adjustment for confounding factors, the odds ratios (95% CI) for mild and severe depressive symptoms when higher green tea consumption was compared with green tea consumption of ≤1 cup/d were as follows: 2–3 cups green tea/d (0.96; 95% CI: 0.66, 1.42) and ≥4 cups green tea/d (0.56; 95% CI: 0.39, 0.81) (P for trend: 0.001). Similar relations were also observed in the case of severe depressive symptoms.
Conclusion
A more frequent consumption of green tea was associated with a lower prevalence of depressive symptoms in the community-dwelling older population.
February 13, 2024
Green tea protects from depression
Dept of Health and Nutrition, Hokkaido University, Japan
Source: J Nutrition Science Vitaminology, Vol 68, 2022
The fact that all studies investigating green tea demonstrate large benefits in preventing depression, and the fact that it is very easy to do, makes this a solid case that adding 2-4 cups of green tea daily should be one of the first strategies for reducing depressive symptoms.
HOW GREEN TEA REDUCES DEPRESSION
As seen in our section on "Abnormalities," people with depression have higher blood markers of body and brain inflammation hormones (neuroinflammation). This includes compounds such as IL-1, IL-6, Tumor Necrosis Factor, C-reactive protein and the marker for oxidative stress malondealdehyde). These inflammaory hormones (which cause the body to think it is under viral assault) results in over-activation of immune cells in the body and brain. This has been shown to lead to elevated cell death in the brain region called the hippocampus (an area that controls memory and mood). Interestingly, one way the brain and body transforms from a normal to inflammatiory state is through abnormalities in our gut bacteria in the small and large intestine, known as the microbiome. Low levels of beneficial gut bacteria and high levels of harmful bacteria have been shown to cause the gut mucus barrier to dissolve and lose its protective function, thereby allowing toxic bacteria in the gut (called LPS) to leak into the blood and cause neuroinflammation and autoimmunity. Scientists call this phenomena "leaky-gut."
In this August 2022 study from South China University of Technology, researchers found a special compound in Green Tea called "epigallocatechin gallate" (EGCG) was able to improve the function of the gut mucus barrier by binding onto mucin (the gel-like particles that make up the gut barrier). Basically working like a glue to hold the remaining mucin together, thereby providing additional strenth to the gut barrier, and reducing the leaky-gut problem. To put this simply, the compound EGCG in Green Tea makes our gut barrier work better - and that's a good thing.
Another way Green Tea may improve depression is that its active compound ECGC has been shown to cross the blood brain barrier and promote new brain cell growth. (link below).
In a very large review of the cellular benefits of EGCG and Green Tea, researchers found it improves cell signaling, reduces early cell death, prevents inflammation by reducing TLR4 receptors and many other benefits related to cancer and other diseases. These studies can be seen by copying and pasting the links below:
Mucin Gut repair
https://pubmed.ncbi.nlm.nih.gov/35768246/
Grows new brain cells
https://pubmed.ncbi.nlm.nih.gov/34443485/
Large review of many benefits of Green Tea
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3909779/
.........................................................
ABSTRACT
This systematic review and meta-analysis aimed to investigate the association between green tea consumption and depression symptom risk, using subgroup analyses concerning study design, geographical region of study, adjustment factors, age, cut-off for the highest consumption category, and depression assessment methods applied. We used PubMed to search for relevant literature. The inclusion criteria were studies that (a) investigated this association as a primary or secondary outcome; (b) published in English; (c) assessed and reported hazard ratios or odds ratios (ORs) and the corresponding 95% confidence intervals (CIs) for depression symptoms, or included sufficient information to allow their calculation; (d) included at least two groups differentiated based on green tea consumption (e.g., high and low); (e) reported the prevalence of depression symptoms in each group; and (f) reported the sample size for each group. Eight articles were found to meet all criteria. The results indicated that high green tea consumption is inversely associated with depression symptoms. The pooled OR was 0.66 (95% CI 0.58-0.74), and significant heterogeneity was not observed. Subgroup analysis showed that study design impacted results (cohort study [one study]: OR=0.29, 95% CI=0.04-2.14; cross-sectional study [seven studies]: OR=0.66, 95% CI=0.59-0.75). These findings suggest that green tea consumption reduces the risk of depression symptoms. This association was also observed in the cohort study included, but the results in which did not reach the significant level. Therefore, further cohort studies are needed to confirm the potential causal relationship in this regard.
February 12, 2024
Probiotics improve depression - increase glutathione & lower CRP
Dept of Psychiatry, Kashan Univ of Med Sciences, Iran
Source: Nutrition, Mar 2016
After completing the 8 week probiotic intervention, patients taking the probiotic supplements had a significantly improved score on the Beck Depression Inventory test (5.7 point improvement) compared with the placebo group. In addition, significant improvements were seen in serum insulin levels, insulin resistance, higher levels of glutathione (an important antioxidant that removes free radicals and typically low in depressed patientss) and lower levels of C-reactive protein (CRP), which is a marker of inflammation and cell death. This study adds to the previous evidence that those with depression have abnormalities with important gut bacteria but can be improved through probiotic supplementation.
..........................................................
ABSTRACT
This randomized, double-blind, placebo-controlled clinical trial included 40 patients with a diagnosis of MDD based on DSM-IV criteria whose age ranged between 20 and 55 y. Patients were randomly allocated into two groups to receive either probiotic supplements (n = 20) or placebo (n = 20) for 8 wk. Probiotic capsule consisted of three viable and freeze-dried strains: Lactobacillus acidophilus (2 × 109 CFU/g), Lactobacillus casei (2 × 109 CFU/g), and Bifidobacterium bifidum (2 × 109 CFU/g). Fasting blood samples were taken at the beginning and end of the trial to quantify the relevant variables. All participants provided three dietary records (two weekdays and one weekend) and three physical activity records during the intervention.
Results
Dietary intake of study participants was not significantly different between the two groups. After 8 wk of intervention, patients who received probiotic supplements had significantly decreased Beck Depression Inventory total scores (−5.7 ± 6.4 vs. −1.5 ± 4.8, P = 0.001) compared with the placebo. In addition, significant decreases in serum insulin levels (−2.3 ± 4.1 vs. 2.6 ± 9.3 μIU/mL, P = 0.03), homeostasis model assessment of insulin resistance (−0.6 ± 1.2 vs. 0.6 ± 2.1, P = 0.03), and serum hs-CRP concentrations (−1138.7 ± 2274.9 vs. 188.4 ± 1455.5 ng/mL, P = 0.03) were observed after the probiotic supplementation compared with the placebo. Additionally, taking probiotics resulted in a significant rise in plasma total glutathione levels (1.8 ± 83.1 vs. −106.8 ± 190.7 μmol/L, P = 0.02) compared with the placebo. We did not find any significant change in fasting plasma glucose, homeostatic model assessment of beta cell function, quantitative insulin sensitivity check index, lipid profiles, and total antioxidant capacity levels.
Conclusions
Probiotic administration in patients with MDD for 8 wk had beneficial effects on Beck Depression Inventory, insulin, homeostasis model assessment of insulin resistance, hs-CRP concentrations, and glutathione concentrations, but did not influence fasting plasma glucose, homeostatic model assessment of beta cell function, quantitative insulin sensitivity check index, lipid profiles, and total antioxidant capacity levels.
February 12, 2024
Vitamin D improves depression in 2 weeks
Dept of Biology Sci & Res Branch, Islamic Azad Univ, Iran
Source: Journal Affective Discordance, May 2020
Prior to beginning the experiment, patients had blood tests measuring serotonin levels and completed the depression severity test known as the Beck Depression Inventory.
After two weeks, the experiment was stopped and patients were given a second blood test and again completed the Beck Depression Inventory. Compared to results prior to beginning vitamin-D, there was a significant 11.75 point improvement in the Beck Depression Inventory, suggesting significantly lower feelings of depression. Blood levels of vitamin-D also increased going from 5.14 (before the test) to 40.83 nmo/L. Interestingly, there was no significant change in blood serotonin levels which the researchers stated suggested the improvement was not mediated by neurotransmitters.
.........................................................
ABSTRACT
Background: Low vitamin D levels are associated with a dysregulated hypothalamic-pituitary-adrenal (HPA) axis and depression but a causal relationship has not been established. This study aimed to evaluate the effects of vitamin D supplementation on depression severity, serum 25(OH)D, and some neurotransmitters in patients with mild to moderate depression.
Methods: An 8-week double-blind randomized clinical trial was conducted on 56 subjects with mild to moderate depression, aged 43.0 ± 1.15yrs. The patients were randomly allocated into two groups: intervention (50,000 IU cholecalciferol/2wks) and control (placebo). Biochemical parameters (serum 25(OH)D, iPTH, oxytocin and platelet serotonin), and depression severity (Beck Depression Inventory-II (BDI-II1)) were initially and finally assessed.
Results: Following intervention, significant changes were observed in the intervention group compared to the controls: 25(OH)D concentrations increased (+40.83±28.57 vs. +5.14±23.44 nmol/L, P<0.001) and BDI scores decreased (-11.75±6.40 vs. -3.61±10.40, P = 0.003). Oxytocin concentrations were significantly reduced in controls (-6.49±13.69 ng/mL, P = 0.01), but between -group differences were insignificant. Within- and between-group differences of platelet serotonin concentrations were not significant; however, the increment in controls was higher (+0.86±10.82 vs. +0.26±9.38 ng/mL, P = 0.83).
Limitations: Study duration may not reflect the long-term effects of vitamin D on depression. It seems necessary to assess tryptophan-hydroxylasetypes1&2 in relation to vitamin D in serotonin pathways.
Conclusions: Eight-week supplementation with 50,000 IU/2wks vitamin D, elevated 25(OH)D concentration of subjects with mild to moderate depression and significantly improved their depression severity. However, there was no evidence that the anti-depressive effect of vitamin D supplementation is mediated by the measured neurotransmitters.
February 10, 2024
Fecal Microbial Transplant (FMT) reverses depression
Dept of Psychiatry, University of Basel, Switzerland
Source: Frontiers in Psychiatry, Feb 2022
To test this possibility, researchers at the University of Basel in Switzerland decided to try an FMT with two patients suffering from major depressive disorder. The first patient, age 53, and the other, age 58, had been treated with antidepressants and psychotherapy with no success, thereby prompting the FMT.
Each patient was given 30 oral frozen FMT capsules over a 90 minute period under the observation of a physician. The 53 year old patient experienced a rapid improvement in symptoms as indicated by a HAMD depression test score going from 21 to 9 in four weeks (an improvement of 11 points). The 58 year old patient experienced an even greater improvement in her HAMD, going from 31 to 10 points after four weeks (an improvement of 21 points). Additionally, two patients given placebos did not improve after four weeks.
In summary, the scientists stated depressive symptoms improved in both patients, going from severe/moderate to mild depression. It was stated that patients with depression are often depleted in butyrate producing bacteria, but the FMT restored this to healthier levels.
...........................................................
ABSTRACT
Depression is a debilitating disorder, and at least one third of patients do not respond to therapy. Associations between gut microbiota and depression have been observed in recent years, opening novel treatment avenues. Here, we present the first two patients with major depressive disorder ever treated with fecal microbiota transplantation as add-on therapy. Both improved their depressive symptoms 4 weeks after the transplantation. Effects lasted up to 8 weeks in one patient. Gastrointestinal symptoms, constipation in particular, were reflected in microbiome changes and improved in one patient. This report suggests further FMT studies in depression could be worth pursuing and adds to awareness as well as safety assurance, both crucial in determining the potential of FMT in depression treatment.
February 9, 2024
Powerful effects of plant terpenoids for improving psychiatric disorders
Agricultural & Life Sci Research, Kangwon Ntl Univ, Korea
Source: Antioxidants, Sep 2022
This would tell us, that any strategy that reduces these inflammatory situations (such as by consuming unique plant compounds) could potentially reverse depression by restoring proper function of the blood brain barrier. For example, the authors state the following plant compounds have been shown to protect the brain from several neurological and cognitive dysfunctions. This includes celastrol, ginsenosides, oleanolic acid, ursoic acid and others. As another example, the compound limonene is a common termpene found in citrus fruits. This was shown to reduce anxiety and increase the metabolic conversion of dopamine and serotonin in the brain area known as the hippocampus and prefrontal cortex. In summary, this easy to read paper provides a scientific basis for using plant compounds (known as neutraceuticals) to improve and potentially reverse depression and other neurological diseases.
..........................................................
ABSTRACT
Terpenoids are widely distributed in nature, especially in the plant kingdom, and exhibit diverse pharmacological activities. In recent years, screening has revealed a wide variety of new terpenoids that are active against different psychiatric disorders. This review synthesized the current published preclinical studies of terpenoid use in psychiatric disorders. This review was extensively investigated to provide empirical evidence regarding the neuropharmacological effects of the vast group of terpenoids in translational models of psychiatric disorders, their relevant mechanisms of action, and treatment regimens with evidence of the safety and psychotropic efficacy. Therefore, we utilized nine (9) electronic databases and performed manual searches of each. The relevant data were retrieved from the articles published until present. We used the search terms “terpenoids” or “terpenes” and “psychiatric disorders” (“psychiatric disorders” OR “psychiatric diseases” OR “neuropsychiatric disorders” OR “psychosis” OR “psychiatric symptoms”). The efficacy of terpenoids or biosynthetic compounds in the terpenoid group was demonstrated in preclinical animal studies. Ginsenosides, bacosides, oleanolic acid, asiatic acid, boswellic acid, mono- and diterpenes, and different forms of saponins and triterpenoids were found to be important bioactive compounds in several preclinical studies of psychosis. Taken together, the findings of the present review indicate that natural terpenoids and their derivatives could achieve remarkable success as an alternative therapeutic option for alleviating the core or associated behavioral features of psychiatric disorders.
February 9, 2024
Natural plant products protect blood brain barrier
Factulty of Pharmacy, University of Sydney, Austrailia
Source: Current Medicinal Chemistry, 2012
ABSTRACT
The blood-brain barrier (BBB) is a protective fence between the central nervous system and the systemic circulation, and is essential for maintaining the normal homeostasis of the central nervous system. BBB breakdown is instigated in many neurological disorders such as Alzheimer's disease and multiple sclerosis. Recent literature has advanced the knowledge on the physiology and pathophysiology of BBB breakdown, including the attribution of detrimental inducers and signalling transduction cascades. Natural products, such as flavonoids, phenolic compounds, terpenes, alkaloids, lipids and phthalides have been reported to attenuate many neurological diseases by modulating the signalling transduction cascades associated with BBB breakdown. Understanding the activities of these natural products through the molecular mechanisms associated with BBB breakdown will offer considerable scope in the discovery and development of novel agents for preventing BBB breakdown and thus, the progression of neurological disorders.
February 8, 2024
Higher fruit & vegetable intake lowers inflammatory CRP
Dept of Human Nutrition, S.B. Univ of Med Sciences, Iran
Source: American J of Clinical Nutrition, Dec 2006
ABSTRACT
Background: Limited data on the relation between the risk of the metabolic syndrome and fruit and vegetable intakes and inflammatory marker concentrations are available.
Objective: We evaluated the relation between fruit and vegetable intakes and C-reactive protein (CRP) concentrations and the prevalence of the metabolic syndrome.
Design: Fruit and vegetable intakes were assessed with the use of a validated semiquantitative food-frequency questionnaire in a cross-sectional study of 486 Tehrani female teachers aged 40-60 y. Anthropometric measurements were made and blood pressure was assessed according to standard methods. Fasting blood samples were taken for biochemical measurements. The metabolic syndrome was defined on the basis of the National Cholesterol Education Program Adult Treatment Panel III guidelines.
Results: The reported mean daily fruit and vegetable intakes were 228 +/- 79 and 186 +/- 88 g/d, respectively. Both fruit and vegetable intakes were inversely associated with plasma CRP concentrations. After statistical control for age, body mass index, and waist circumference, mean plasma CRP concentrations across increasing quintile categories of fruit intakes were 1.94, 1.79, 1.65, 1.61, and 1.56 mg/L and of vegetable intakes were 2.03, 1.82, 1.58, 1.52, and 1.47 mg/L (P for trend < 0.01 for both). These inverse associations remained significant after additional control for other potential confounding variables and dietary factors. After control for potential confounders, persons in the highest quintile of fruit intake had a 34% (95% CI: 20%, 46%) lower and those in the highest quintile of vegetables intake had a 30% (95% CI: 16%, 39%) lower chance of having the metabolic syndrome than did those in the lowest quintiles.
Conclusions: Higher intakes of fruit and vegetables are associated with a lower risk of the metabolic syndrome; the lower risk may be the result of lower CRP concentrations. These findings support current dietary recommendations to increase daily intakes of fruit and vegetables as a primary preventive measure against cardiovascular disease.
February 8, 2024
Organic food appears important to reverse depression (lowers CRP)
School of Pub Health, Univ of Michigan
Source: Public Health nutrition, Oct 2021
However most people today are unfortunately around 1.5-1.8 mg/dL (15-18 mg/L. Those with depressive disorder are often over 2.5 mg/dL (25 mg/L) and anything from 3.0 (30 mg/L) and higher is considered high and evidence of damaging chronic inflammation and higher risk of heart attack. Scientists at University of Michigan found a simple way each of us can quickly reduce our CRP and the damaging brain and body inflammation that goes with it.
EAT ORGANIC
Organically grown food contains far lower levels of pesticide residues as well as 50% lower levels of the toxic metal cadminum (which is concentrated in chemical fertilizer processing). These toxic chemicals can damage tissues, thereby increasing inflammation and CRP. While many environmental factors have been identified that increase CRP, the switch to organic food to reduce CRP should be easy to achieve. Researchers stated, even after adjusting for all confounding factors, those eating organic food had significantly lower levels of C-reactive protein.
............................................................
ABSTRACT
Objective:
The association between organic food consumption and biomarkers of inflammation, C-reactive protein (CRP) and cystatin C (CysC) was explored in this cross-sectional analysis of older adults.
Design:
Dietary data and organic food consumption was collected in 2013 from a FFQ. Alternative Mediterranean diet score (A-MedDiet) was calculated as a measure of healthy eating. Biomarkers CRP and CysC were collected in serum or plasma in 2016. We used linear regression models to assess the associations between organic food consumption and CRP and CysC.
Setting:
This cross-sectional analysis uses data from the nationally representative, longitudinal panel study of Americans over 50, the Health and Retirement Study.
Participants:
The mean age of the analytic sample (n 3815) was 64·3 (se 0·3) years with 54·4 % being female.
Results:
Log CRP and log CysC were inversely associated with consuming organic food after adjusting for potential confounders (CRP: β = –0·096, 95 % CI 0·159, –0·033; CysC: β = –0·033, 95 % CI –0·051, –0·015). Log CRP maintained statistical significance (β = –0·080; 95 % CI –0·144, –0·016) after additional adjustments for the A-MedDiet, while log CysC lost statistical significance (β = –0·019; 95 % CI –0·039, 0·000). The association between organic food consumption and log CRP was driven primarily by milk, fruit, vegetables and cereals, while log CysC was primarily driven by milk, eggs and meat after adjustments for A-MedDiet.
Conclusions:
These findings support the hypothesis that organic food consumption is inversely associated with biomarkers of inflammation CRP and CysC, although residual confounding by healthy eating and socioeconomic status cannot be ruled out.
February 8, 2024
Diet sweetener aspartame damages brain - decreases serotonin
Dept of Animal Anatomy & Histology, Univ of Life Sci, Poland
Source: Folia Neuropathology, Mar 2013
ABSTRACT
Aspartame, a widespread sweetener used in many food products, is considered as a highly hazardous compound. Aspartame was discovered in 1965 and raises a lot of controversy up to date. Astrocytes are glial cells, the presence and functions of which are closely connected with the central nervous system (CNS). The aim of this article is to demonstrate the direct and indirect role of astrocytes participating in the harmful effects of aspartame metabolites on neurons.
The artificial sweetener is broken down into phenylalanine (50%), aspartic acid (40%) and methanol (10%) during metabolism in the body. The excess of phenylalanine blocks the transport of important amino acids to the brain contributing to reduced levels of dopamine and serotonin. Astrocytes directly affect the transport of this amino acid and also indirectly by modulation of carriers in the endothelium. Aspartic acid at high concentrations is a toxin that causes hyperexcitability of neurons and is also a precursor of other excitatory amino acid - glutamates. Their excess in quantity and lack of astrocytic uptake induces excitotoxicity and leads to the degeneration of astrocytes and neurons.
The methanol metabolites cause CNS depression, vision disorders and other symptoms leading ultimately to metabolic acidosis and coma. Astrocytes do not play a significant role in methanol poisoning due to a permanent consumption
of large amounts of aspartame.
Despite intense speculations about the carcinogenicity of aspartame, the latest studies show that its metabolite – diketopiperazine – is cancirogenic in the CNS. It contributes to the formation of tumors in the CNS such as gliomas, medulloblastomas and meningiomas. Glial cells are the main source of tumors, which can be caused inter alia by the sweetener in the brain.
On the one hand the action of astrocytes during aspartame poisoning may be advantageous for neuro-protection while
on the other it may intensify the destruction of neurons. The role of the glia in the pathogenesis of many CNS diseases is crucial.
February 7, 2024
Non-Drug treatments for Depression
Dept of Clnical Sci, Psychiatry, Lund Univ, Sweden
Source: Int J of Molecular Science, Feb 2021
Continue reading below....
Scientists also review studies showing depression can be improved by exercise, fecal microbiota transplant and probiotics. Interestingly, patients with depressive disorder are repeatedly shown to have an abnormal gut bacteria (called dysbiosis). For example, depressed patients were shown to have lower quality of the beneficial gut bacteria Lactobacillus. Many of these bacteria are involved in suppressing inflammation and increasing production of serotonin and dopamine, thereby providing a basis why treating gut health may be the most important tool for reversing depression and improving symptoms.
......................................
ABSTRACT
Treatment of depression is hampered by the failure to identify distinct symptom profiles with distinct pathophysiologies that differentially respond to distinct treatments. We posit that inflammatory depression is a meaningful depression subtype associated with specific symptoms and biological abnormalities. We review several upstream, potentially causative, mechanisms driving low-grade inflammation in this subtype of depression. We also discuss downstream mechanisms mediating the link between inflammation and symptoms of depression, including alterations in dopaminergic neurotransmission and tryptophan metabolism. Finally, we review evidence for several non-pharmacological interventions for inflammatory depression, including probiotics, omega-3 fatty acids, and physical exercise interventions. While some evidence suggests that these interventions may be efficacious in inflammatory depression, future clinical trials should consider enriching patient populations for inflammatory markers, or stratify patients by inflammatory status, to confirm or refute this hypothesis.
February 4, 2024
Reverse depression by improving microbiome, intestinal barrier & probiotics
Chair & Dept of Toxic, Medical Univ, Lublin
Source: Nutrients, Mar 2021
ABSTRACT
The intestinal microbiota plays an important role in the pathophysiology of depression. As determined, the microbiota influences the shaping and modulation of the functioning of the gut–brain axis. The intestinal microbiota has a significant impact on processes related to neurotransmitter synthesis, the myelination of neurons in the prefrontal cortex, and is also involved in the development of the amygdala and hippocampus. Intestinal bacteria are also a source of vitamins, the deficiency of which is believed to be related to the response to antidepressant therapy and may lead to exacerbation of depressive symptoms. Additionally, it is known that, in periods of excessive activation of stress reactions, the immune system also plays an important role, negatively affecting the tightness of the intestinal barrier and intestinal microflora. In this review, we have summarized the role of the gut microbiota, its metabolites, and diet in susceptibility to depression. We also describe abnormalities in the functioning of the intestinal barrier caused by increased activity of the immune system in response to stressors. Moreover, the presented study discusses the role of psychobiotics in the prevention and treatment of depression through their influence on the intestinal barrier, immune processes, and functioning of the nervous system.
February 4, 2024
Healthy lifestyle reduces neuroinflammation & prevents neurological disorders
Dept of Anatomy, Univ of Otago, New Zealand
Source: Frontiers Neuroscience, Feb 2023
ABSTRACTSince the mid-20th century, Western societies have considered productivity and economic outcomes are more important than focusing on people’s health and wellbeing. This focus has created lifestyles with high stress levels, associated with overconsumption of unhealthy foods and little exercise, which negatively affect people’s lives, and subsequently lead to the development of pathologies, including neurodegenerative and psychiatric disorders. Prioritizing a healthy lifestyle to maintain wellbeing may slow the onset or reduce the severity of pathologies. It is a win-win for everyone; for societies and for individuals. A balanced lifestyle is increasingly being adopted globally, with many doctors encouraging meditation and prescribing non-pharmaceutical interventions to treat depression. In psychiatric and neurodegenerative disorders, the inflammatory response system of the brain (neuroinflammation) is activated. Many risks factors are now known to be linked to neuroinflammation such as stress, pollution, and a high saturated and trans fat diet. On the other hand, many studies have linked healthy habits and anti-inflammatory products with lower levels of neuroinflammation and a reduced risk of neurodegenerative and psychiatric disorders. Sharing risk and protective factors is critical so that individuals can make informed choices that promote positive aging throughout their lifespan. Most strategies to manage neurodegenerative diseases are palliative because neurodegeneration has been progressing silently for decades before symptoms appear. Here, we focus on preventing neurodegenerative diseases by adopting an integrated “healthy” lifestyle approach. This review summarizes the role of neuroinflammation on risk and protective factors of neurodegenerative and psychiatric disorders.
January 24, 2024
Raising body temperature improves depression
International J of Hyperthermia, April 2019
Source: Dept of Psychology, University of Arizona
ABSTRACT
Objective: To systematically summarize the findings from research studies examining the effects of whole-body hyperthermia (WBH) interventions on mood and symptoms of depression.
Methods: Systematic literature search of online and offline databases (e.g., Pubmed, Web of Knowledge, Cochrane, academic libraries). Risk of bias assessment and secondary analysis of effect sizes.
Study selection: Clinical studies with a pre/post-intervention design and outcome measures for mood and depression as accepted in the S-3 guidelines (Association of Scientific Medical Societies in Germany).
Data extraction: Study characteristics and outcomes (means and standard deviations) from participants receiving at least one WBH intervention.
Results: A total of 7 studies and 148 subjects with a mean age of 46 years (36–56 years) were identified. Three out of seven studies utilized hot baths and 4/7 infrared heating. Study duration ranged from 1 to 6 weeks with one or multiple interventions and an average treatment time of 66.37 min (42.55–140). Risk of bias analysis revealed small sample biases and lack of control groups in 3/7 studies. About 21 study end-points were extracted with 19 resulting in effects sizes (Cohen’s d) of 0.8 or greater. Target temperatures between 38 °C and 39 °C and slower increase in core body temperature during the intervention resulted in larger treatment effects.
Conclusion: WBH is a promising alternative treatment for depression with low risk for adverse reactions and side effects but still lacking sufficient evidence for general recommendations for clinical practice. However, as all other interventions have failed, the studies to date can provide a framework for clinical application.
January 22, 2024
Bipolar Disorder abnormalities in gut microbiome - Improved by FMT
Dept Neurosciences, Univ G.D'Annunzio, Italy
Source: International J Molecular Science, Apr 2021
The gut microbiota is the set of microorganisms that colonize the gastrointestinal tract of living creatures, establishing a bidirectional symbiotic relationship that is essential for maintaining homeostasis, for their growth and digestive processes. Growing evidence supports its involvement in the intercommunication system between the gut and the brain, so that it is called the gut–brain–microbiota axis. It is involved in the regulation of the functions of the Central Nervous System (CNS), behavior, mood and anxiety and, therefore, its implication in the pathogenesis of neuropsychiatric disorders. In this paper, we focused on the possible correlations between the gut microbiota and Bipolar Disorder (BD), in order to determine its role in the pathogenesis and in the clinical management of BD. Current literature supports a possible relationship between the compositional alterations of the intestinal microbiota and BD. Moreover, due to its impact on psychopharmacological treatment absorption, by acting on the composition of the microbiota beneficial effects can be obtained on BD symptoms. Finally, we discussed the potential of correcting gut microbiota alteration as a novel augmentation strategy in BD. Future studies are necessary to better clarify the relevance of gut microbiota alterations as state and disease biomarkers of BD.
January 20, 2024
Whole coffee cherry extract improves BDNF & brain function
Dept Psychiatry, Auburn
Source: UniversityAntioxidants, Feb 2021
ABSTRACT
Bioactive plant-based compounds have shown promise as protective agents across multiple domains including improvements in neurological and psychological measures. Methodological challenges have limited our understanding of the neurophysiological changes associated with polyphenol-rich supplements such as whole coffee cherry extract (WCCE). In the current study, we (1) compared 100 mg of WCCE to a placebo using an acute, randomized, double-blind, within-subject, cross-over design, and we (2) conducted a phytochemical analysis of WCCE. The primary objective of the study was to determine the neurophysiological and behavioral changes that resulted from the acute administration of WCCE. We hypothesized that WCCE would increase brain-derived neurotrophic factor (BDNF) and glutamate levels while also increasing neurofunctional measures in cognitive brain regions. Furthermore, we expected there to be increased behavioral performance associated with WCCE, as measured by reaction time and accuracy. Participants underwent four neuroimaging scans (pre- and post-WCCE and placebo) to assess neurofunctional/metabolic outcomes using functional magnetic resonance imaging and magnetic resonance spectroscopy. The results suggest that polyphenol-rich WCCE is associated with decreased reaction time and may protect against cognitive errors on tasks of working memory and response inhibition. Behavioral findings were concomitant with neurofunctional changes in structures involved in decision-making and attention. Specifically, we found increased functional connectivity between the anterior cingulate and regions involved in sensory and decision-making networks. Additionally, we observed increased BDNF and an increased glutamate/gamma-aminobutyric acid (GABA) ratio following WCCE administration. These results suggest that WCCE is associated with acute neurophysiological changes supportive of faster reaction times and increased, sustained attention.
December 11, 2023
Mushrooms show promise for treating depression
School of Biomedical Sci, Univ of Hong Kong
Source: Int J Molecular Science, Jan 2020
ABSTRACT
Depression is a common and severe neuropsychiatric disorder that is one of the leading causes of global disease burden. Although various anti-depressants are currently available, their efficacies are barely adequate and many have side effects. Hericium erinaceus, also known as Lion’s mane mushroom, has been shown to have various health benefits, including antioxidative, antidiabetic, anticancer, anti-inflammatory, antimicrobial, antihyperglycemic, and hypolipidemic effects. It has been used to treat cognitive impairment, Parkinson’s disease, and Alzheimer’s disease. Bioactive compounds extracted from the mycelia and fruiting bodies of H. erinaceus have been found to promote the expression of neurotrophic factors that are associated with cell proliferation such as nerve growth factors. Although antidepressant effects of H. erinaceus have not been validated and compared to the conventional antidepressants, based on the neurotrophic and neurogenic pathophysiology of depression, H. erinaceus may be a potential alternative medicine for the treatment of depression. This article critically reviews the current literature on the potential benefits of H. erinaceus as a treatment for depressive disorder as well as its mechanisms underlying the antidepressant-like activities.
September 17, 2023
Omega-3 fatty acids improve blood brain barrier
Dept of Radiology, Loma Linda University California
Source: Brain & Behavior, Aug 2021
A component found in Omega-3 is called EPA, which was stated by the scientists to reduce neuroinflammation, which as stated in our Abnormality section, is higher in those with depression. This would suggest the addition of Omega-3 would be advantageous for those with depression.
ABSTRACT
In aging populations, omega-3 polyunsaturated fatty acids (PUFAs) have been associated with better cognitive function, slower rates of cognitive decline, and lower risk of developing dementia. Animal studies have shown that diets rich in omega-3 PUFAs reduce blood-brain barrier (BBB) disruption associated with aging, but this has yet to be observed in humans. Forty-five healthy subjects (mean age, 76 years) were recruited and underwent cognitive assessment (verbal learning and memory, language, processing speed, executive function, and motor control) and measurement of PUFAs. Forty of the same subjects also underwent magnetic resonance imaging (MRI) to measure BBB integrity (Ktrans using dynamic contrast-enhanced MRI). The long chain omega-3 score (DHA+EPA) was negatively correlated with Ktrans values in the internal capsule, indicating higher omega-3 levels were associated with greater BBB integrity in this region (r = -0.525, p = .004). Trends were observed for a positive correlation between the long chain omega-3 score and both memory and language scores, but not with executive function, speed, or motor control. The omega-6 score was not significantly correlated with any cognitive scores or Ktrans values. The significant correlations between long chain omega-3 levels and BBB integrity provide a possible mechanism by which omega-3 PUFAs are associated with brain health.
September 16, 2023
Omega-3 reverses depression in unique ways
Psychiatry & Imunology, Kings College, London
Source: Molecular Psychiatry, Jun 16 2021
ABSTRACT
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) can exert antidepressant, anti-inflammatory and neuroprotective properties, but the exact molecular mechanism underlying their effects is still not fully understood. We conducted both in vitro and clinical investigations to test which EPA or DHA metabolites are involved in these anti-inflammatory, neuroprotective and antidepressant effects. In vitro, we used the human hippocampal progenitor cell line HPC0A07/03C, and pre-treated cells with either EPA or DHA, followed by interleukin 1beta (IL1β), IL6 and interferon-alpha (IFN-α). Both EPA and DHA prevented the reduction in neurogenesis and the increase in apoptosis induced by these cytokines; moreover, these effects were mediated by the lipoxygenase (LOX) and cytochrome P450 (CYP450) EPA/DHA metabolites, 5-hydroxyeicosapentaenoic acid (HEPE), 4-hydroxydocosahexaenoic acid (HDHA), 18-HEPE, 20-HDHA, 17(18)-epoxyeicosatetraenoic acid (EpETE) and 19(20)-epoxydocosapentaenoic acid (EpDPA), detected here for the first time in human hippocampal neurones using mass spectrometry lipidomics of the supernatant. In fact, like EPA/DHA, co-treatment with these metabolites prevented cytokines-induced reduction in neurogenesis and apoptosis. Moreover, co-treatment with 17(18)-EpETE and 19(20)-EpDPA and the soluble epoxide hydroxylase (sEH) inhibitor, TPPU (which prevents their conversion into dihydroxyeicosatetraenoic acid (DiHETE)/ dihydroxydocosapentaenoic acid (DiHDPA) metabolites) further enhanced their neurogenic and anti-apoptotic effects. Interestingly, these findings were replicated in a sample of n = 22 patients with a DSM-IV Major Depressive Disorder, randomly assigned to treatment with either EPA (3.0 g/day) or DHA (1.4 g/day) for 12 weeks, with exactly the same LOX and CYP450 lipid metabolites increased in the plasma of these patients following treatment with their precursor, EPA or DHA, and some evidence that higher levels of these metabolites were correlated with less severe depressive symptoms. Overall, our study provides the first evidence for the relevance of LOX- and CYP450-derived EPA/DHA bioactive lipid metabolites as neuroprotective molecular targets for human hippocampal neurogenesis and depression, and highlights the importance of sEH inhibitors as potential therapeutic strategy for patients suffering from depressive symptoms.
September 15, 2023
Curcumin highly effective for treating depression & anxiety
Murdoch University, Australia
Source: CNS Drugs, Feb 7 2022
ABSTRACT
Curcumin is the major biologically active polyphenolic constituent in the turmeric plant (Curcuma longa) that has been shown to have antioxidant, anti-inflammatory, neuroprotective, anticancer, antimicrobial, and cardioprotective effects. Interest in curcumin as a treatment for mental health conditions has increased and there is an expanding body of preclinical and clinical research examining its antidepressant and anxiolytic effects. In this narrative review, human trials investigating the effects of curcumin for the treatment of depression or depressive symptoms are summarised. Using findings from in vitro, animal, and human trials, possible biological mechanisms associated with the antidepressant effects of curcumin are also explored. To increase the understanding of curcumin for the treatment of depression, directions for future research are proposed.
January 19, 2020
Plant compounds activate neurogenesis (new brain cell growth)
Inst of Psychiatry, King's College, London
Source: Oxidation Med Cell Longevity, Jun 2012
ABSTRACT
Although it has been long believed that new neurons were only generated during development, there is now growing evidence indicating that at least two regions in the brain are capable of continuously generating functional neurons: the subventricular zone and the dentate gyrus of the hippocampus. Adult hippocampal neurogenesis (AHN) is a widely observed phenomenon verified in different adult mammalian species including humans. Factors such as environmental enrichment, voluntary exercise, and diet have been linked to increased levels of AHN. Conversely, aging, stress, anxiety and depression have been suggested to hinder it. However, the mechanisms underlying these effects are still unclear and yet to be determined. In this paper, we discuss some recent findings addressing the effects of different dietary polyphenols on hippocampal cell proliferation and differentiation, models of anxiety, and depression as well as some proposed molecular mechanisms underlying those effects with particular focus on those related to AHN. As a whole, dietary polyphenols seem to exert positive effects on anxiety and depression, possibly in part via regulation of AHN. Studies on the effects of dietary polyphenols on behaviour and AHN may play an important role in the approach to use diet as part of the therapeutic interventions for mental-health-related conditions.
Those with depression (depressive disorder) typically have higher rates of secondary health problems. The reasons for this appear related to the higher levels of inflammation markers common with depression (including higher Interleukin 1, Interleukin-6, Tumor Necrosis Factor and sometimes shown as high C-reactive protein). Higher inflammatory markers acclerate damage and normal function of cells in the heart, blood vessels, adipose tissue (obesity), pancreas (diabetes) and other organs. This fact stresses the importance of attempting to treat the cause of depression at the onset rather than the symptoms.
February 18, 2024
Arthritis higher in depression - easily explained
Psychiatry Dept, Univ Hospital of St Etienne, FR
Source: Joint Bone Spine, Oct 2021
ABSTRACT
Depression constitutes the most frequent comorbid condition associated with rheumatoid arthritis (RA), with prevalence rates ranging from 14% to 48%. This wide range can be explained by several factors including subtypes of depression considered, instrument of measure (i.e. self-questionnaires versus clinical interview), threshold applied but also the overlap of symptoms between the two conditions. Despite being a frequent comorbid condition in RA, depressive states are repeatedly underdiagnosed and thus, often remain untreated. Consequences are dramatic as conclusive evidence show that depression deleteriously impacts just about all outcomes of RA, including disease activity, arthritis-related complications, level of pain, chance of remission, quality of life and mortality. Importantly, links between depression and RA appear to be bidirectional as if RA patients show increased prevalence of depression. Conversely, patients with depression compared to the general population have higher risk to develop RA. Among the factors explaining this strong association between depression and RA, recent advances have underlined the putative role of models based on the inflammatory hypothesis. Pro-inflammatory cytokines such as tumor necrosis factor, interleukin (IL)-1, IL-6, and IL-18 are involved in RA pathogenesis, but also in depression. Furthermore, the connections between the central nervous system, the peripheral system and the immune system are now better understood. As a consequence of the strong comorbidity and the aggravate prognostic, the management of patient showing this dual diagnosis should be carefully monitor. The common physiopathology also opens the path to utilization of RA treatment in severe depression or treatment-resistant depression.
February 7, 2024
Additional health problems in women with depression
Dept of Obst and Gyn, Korea Univ Anam Hospital
Source: Medicina, Dec 2023
The risk for stroke was 170% higher and risk of heart attack was over 700% higher, when compared to women without depression. These are dramatic differences and would appear to be related to the increased levels of inflammation markers (including interleukin-6 and C-reactive protein) that not only harm the brain, but can accelerate aging and damage to other body tissues as well. These numbers stress the importance at locating the biological cause for the person's depression, before looking into pharmaceutical treatments shown to be only marginally effective and come with additional side effects.
...........................................................
ABSTRACT
Background and Objectives: Serum vitamin levels, cardiovascular disease risk factors, and their association with depression is a complex issue that has been the subject of much research. Therefore, we investigated the relationship between vitamin A, B9, and E levels, cardiovascular risk factors, and depression in premenopausal and menopausal South Korean women. Materials and Methods: This cross-sectional study used the 2016–2018 Korea National Health and Nutrition Examination Survey data. Depression was assessed using a questionnaire to check for symptoms of depression or the Patient Health Questionnaire–9. Blood samples were collected from the antecubital vein in the morning after an overnight fast. Covariates were defined as self-reported physician diagnoses. Well-trained medical staff performed the standard procedures. Statistical analysis was performed using the complex sample analysis method of SPSS, using two separate logistic regression models (model 1: adjusted for age; model 2: adjusted for age, marital status, smoking, and alcohol consumption). Results: A total of 3313 women aged over 20 years were enrolled. The association between vitamin A levels and depression was as follows: lower levels of vitamin A were associated with an increased risk of depression in premenopausal women in model 1 and model 2. The levels of serum vitamins E and B9 were not correlated with depression in premenopausal and postmenopausal women. In the premenopausal group, depression increased in the obesity (model 1: p = 0.037; model 2: p = 0.047) and diabetes mellitus (model 1: p = 0.010; model 2: p = 0.009) groups. The menopausal group with depression had higher rates of stroke (model 1: p = 0.017; model 2: p = 0.039) and myocardial infarction (model 1: p = 0.004; model 2: p = 0.008) than the group without depression. Conclusions: Depression is correlated with lower blood levels of vitamin A in premenopausal women. Vitamin B9 and E levels were not associated with depression independent of menopausal status. Depression is associated with obesity and diabetes mellitus in premenopausal women and with stroke and myocardial infarction in postmenopausal women.
February 4, 2024
Heart problems high in patients with depressive disorder
Cntr for Indigenous Vasc & Diabetes Res, Australia
Source: CNS Drugs, Vol 23(7) 2009
ABSTRACT
This article provides a detailed review of the association of major depression with coronary heart disease (CHD), examines the biological variables underpinning the linkage and discusses the clinical implications for treatment. When considering the co-morbidity between major depressive disorder (MDD) and CHD it is important to differentiate between (i) the prevalence and impact of MDD in those with existing CHD and (ii) MDD as a risk factor for the development of CHD. Whether the same biological mechanisms are at play in these two instances remains unknown. Depression is common in patients with CHD. Importantly, depression in these patients increases mortality. There is also consistent evidence that MDD is a risk factor for the development of CHD. The relative risk of developing CHD is proportional to the severity of depression and is independent of smoking, obesity, hypercholesterolaemia, diabetes mellitus and hypertension. There is a clear need to identify the underlying neurochemical mechanisms responsible for MDD and their linkage to the heart and vascular system. Of particular interest are activation of stress pathways, including both the sympathetic nervous system and hypothalamic-pituitary-adrenal axis, and inflammatory-mediated atherogenesis. Elevated sympathetic activity, reduced heart rate variability and increased plasma cortisol levels have been documented in patients with MDD. In addition to direct effects on the heart and vasculature, activation of stress pathways may also be associated with increased release of inflammatory cytokines such as interleukin-6 and tumour necrosis factor-alpha. Elevated levels of C-reactive protein are commonly observed in patients with MDD. The majority of investigations examining treatment of depression following myocardial infarction have focused on safety and efficacy; there is little evidence to indicate that treating depression in these patients improves survival. Given that strategies for preventive therapy remain incompletely formulated, future research should focus on generating a better understanding of the neurobiology of MDD and heart disease as a basis for rational and effective therapy.
View another category from the menu above.